Positive Health Online
Your Country

Mindfulness and the Breath
by Dr David Beales and Jonathan Nunn(more info)
listed in breathing, originally published in issue 183 - June 2011
A Doctor and an Osteopath share their combined thoughts on the way the breath plays a central role in restoring and maintaining health and vitality.
Breathless with Excitement:
For most of the time we are not conscious of how we breathe at all. It is only when we become ‘breathless with excitement’ or stop before a beautiful view and in amazement perhaps ‘hold our breath’ that we become consciously aware of our breath breathing us.
Working together:
Osteopath Jonathan Nunn and holistic Medical Doctor David Beales both find, in their different professions, that how we breathe is of fundamental importance in maintaining health, well being and spiritual connection.
David works as a specialist in behavioural medicine, resolving symptoms produced by mind-body imbalance such as anxiety, depression and functional ill health when individuals reach the limit of their tolerance to life challenges. Jonathan, as a busy Osteopath, resolves body-mind discord manifesting in back pain and muscular tension as reactions to injury and/or stress. They both work with the breath. They add mindfulness practice defined by Thich Naht Hahn as ‘the capacity to be aware of what is going on moment by moment’[1] - an essential ingredient of their own enjoyable lives.
Teaching together:
They initially met at Hawkwood College, a dynamic centre of adult education near Stroud, Gloucestershire where Jonathan attended David’s course called “Creating Health: Mind/Body Medicine and Meditation.” “The course brought so much together for me and when others assumed I was teaching it because of my long term interest in the breath, I realized it was time to develop my own approach,” says Jonathan. Now they teach together at Hawkwood and are preparing for their 2011 course taking place on Saturday 30th and Sunday 31st July. “This is an exciting time to collaborate and help participants understand the many aspects of breathing; as well as to find the right practices to optimise energy and reduce or eliminate the effects of physical or emotional dis-ease,” says David.
Breathing Re-training and Mindfulness:
A central platform of mindfulness is paying attention to the breath as it moves in and out moment to moment. You will learn the ability to return to the ‘Now of present moment awareness’ as described by Erkhart Toll.[2] This ability then allows you to regain present moment awareness and re-connect with yourself without thinking.
Creating a breathing space in the midst of stress is a central plank of mindfulness based cognitive behavioural therapy. Eight 2 hourly sessions have been shown to be a very effective vehicle for recovery after three or more severe episodes of depression. [3] The persistence of unchallenged negative thought, creates a mind-body groove in the brain’s neural pathways; the breathing space ‘lifts the energy and impact of the negative emotion from the neural pathways at the contact point’ thereby allowing new circuitry to develop.
Recent research at King’s College London reported in Science review has shown how antidepressant drugs activate a key protein involved in the brain’s response to stress called the glucocorticoid receptor. The drugs stimulate new brain cells a process called neurogenesis.[5] A similar mechanism may be the reason that meditation and cognitive behavioural therapy are effective in depression. The approaches taught allow new pathways within the brain to re-activate. They are made permanent by new behaviours associated with positive emotional states. [4]
Breathing and Body Chemistry:
How we breathe can profoundly affect the chemistry of the body by altering its PH value or acidity levels as well as reducing the release of available oxygen to cells.[6] David works with capnography, using a small device that measures the amount of carbon dioxide levels in the exhalation. (The main application of capnography is in monitoring carbon dioxide levels occurs when an anaesthetist inserts a breathing tube during anaesthesia. The presence of carbon dioxide confirms that the tube is correctly placed within the lung, as there is only a small amount of this gas in ordinary air.) Capnotraining software programmes enable participants to see carbon dioxide directly on the computer screen. You will be able to see whether your present breathing style at rest and with different breathing rates or whilst imagining situation challenges produces the right carbon dioxide levels. This approach demonstrates directly the evidence if present of prolonged or intermittent over-breathing. Then levels of carbon dioxide fall from normal values where the threshold at rest is set at 35mm of partial pressure of Mercury. Below 35 mm to 30 mm of Hg suggests mild to moderate overbreathing and hypocapnia (reduced carbon dioxide levels). Below 30 mm of Hg suggests chronic over breathing.
Over breathing reduces carbon dioxide and oxygen flow:
For a drop in partial pressure of carbon dioxide of 2mm - from the normal of 38-40 mm partial pressure of Mercury - the body’s Haemoglobin will hold onto 2% of Oxygen without releasing oxygen to cells within the body – The Bohr Effect.[6]
A reduction from 40 mm to 20 mm results in a 40% fall in oxygen release. A reasonable hypothesis to explain a dominant symptom of chronic over breathing, such as difficulty in maintaining normal contact with your surroundings, creating ‘brain fog’ can be explained by this mechanism as well as many other often medically unexplained symptoms accounting for up to 30% of all GP Consultations.[7]
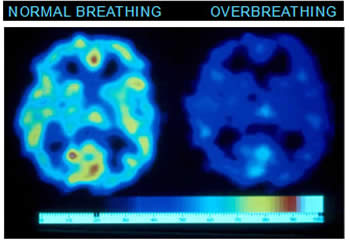
Magnetic resonance brain scan demonstrating oxygen release.
The connection of Over Breathing with Stress and ‘Fight Flee or Freeze’:
When under stress the breathing pattern changes. Typically, an anxious person takes small, shallow breaths, raising their shoulders and using upper chest muscles rather than their diaphragm to move air in and out of their lungs. This style of breathing moves too much carbon dioxide out of the air passages and blood than is being made by the normal metabolism of the body and upsets the balance of gases. If the stressful situation is not resolved and chronic over breathing results many symptoms can occur in multiple body systems such as:[9]
- Chest tightness, chest pains and tension
- Dizziness, brain fog and losing contact with normal surroundings
- Breathing symptoms such as rapid or deep breathing
- Difficulties taking a deep breath, shortness of breath and difficulty breathing
- Feelings of panic and anxiety
- Colds hands and feet and/or tingling of the fingers
- Heart palpitations
- Muscular stiffness and/or a perception of tightness around the mouth
- A bloated abdomen
As carbon dioxide levels fall, small blood vessels in the skin with smooth muscle in their walls called arterioles constrict, causing blood to be diverted into the larger blood vessels deep within muscles as resistance to the hearts cardiac output is raised. This has been designed to aid the ‘get away’ or the ‘withdrawal’ (flight/fight/freeze) response diverting blood to muscles and also to our emotional brain deep within the limbic system. Hypertension can result and a device called a Resperate that slows the breathing rate and prolongs the out breath is evidence based and recommended by doctors.[9]
Bronchioles – the small air passages in the lungs may constrict and this can result in asthma.[16]
Client Report: Jo attended a workshop and described intermittent episodes of coughing and wheezing that were interfering with her preparation for an important professional exam. At the beginning of the workshop she had no symptoms and showed normal levels of carbon dioxide of 40mm partial pressure of Mercury. She was asked to over breath whilst carbon dioxide in the out breath was monitored. When she reached 23 mm of Mercury her cough returned. As she restored carbon dioxide levels she lost her symptoms. As she over breathed symptoms returned. She remembered that each time during her life that she had been taking an exam she developed symptoms of cough and wheeze. As she made the connection between how she breathed under stress and her symptoms she recognized that mindful watching for the first signals of over breathing will help her manage her asthma better. Careful monitoring of her asthma and the use of a combination of inhaler medication and breath awareness is now more effective for her.
Research has led to the recommendation for breathing re-training by the National Institute for Clinical Excellence (NICE) for people with asthma.[11]
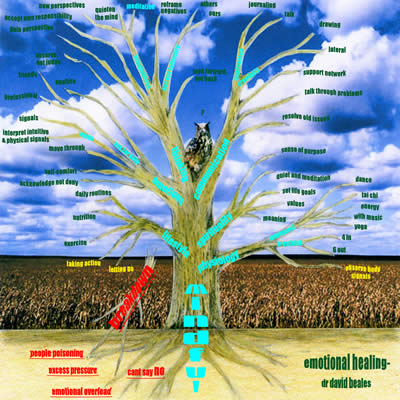
Emotional Healing:
The brain’s emotional centres open when under stress to help you pattern match to previous similar episodes of stress. The over-breathing response is carried over as part of your threat response from the time when you needed to become aware of danger. Survival depended on responding to the signals of the approaching sabre-toothed tiger but become less helpful in responding to major concerns about how to pay the mortgage! David and his partner Helen Whitten describe in Emotional Healing for Dummies a comprehensive programme to recover emotional resilience.[12]
Five Step Emotional Healing Process © Wiley / David Beales & Helen Whitten
Step 1: Identify Disturbing Situation
Step 2: Notice Distress Signals:
- Physical symptoms and breath signals
- Upset emotions
- Disturbed Thinking
- Unhelpful Behaviours
Step 3: Take a Breathing Space:
- Stop, Step Back, Calm Body-Mind.
Step 4: Release Pressure to Regain Control
- Relax body and apply breath to restore C02
- Choose a helpful emotional state
- Focus on constructive thoughts
- Question: What did I do?
- What do I need to do now?
- Choose appropriate behaviour: Speak up and Act as you need
Step 5: Embrace change, Rehearse, Review, Embed new Behaviours in Action

John’s Story: John came to the clinic having been diagnosed with the chronic hyperventilation syndrome at the Brompton Hospital. He had typically low levels of carbon dioxide at rest of the order of 25mm of Mercury. He had been unable to work for four months and despite two episodes of treatment with respiratory physiotherapists remained with many symptoms and marked anxiety. A validated questionnaire for the chronic hyperventilation syndrome – the Nijmegen Questionnaire consisting of 16 questions[9] – has a specificity of 93% and a reliability of 91%. He scored 56 (Scores above 23 are predictive). Leading up to the diagnosis he was increasingly troubled by a variety of body mind symptoms ranging from tension and anxiety to abdominal bloating and difficulty in concentrating. He had also been in the midst of severe family stress after the death of his father. He recovered after breathing re-training, using carbon dioxide feedback, where he was able to regain accuracy in breathing behaviour that allowed him to restore good carbon dioxide levels and notice the situations where his breathing chemistry was disturbed. The 5 step process as described above was combined with cognitive behavioural coaching. He returned to work.
How to retain or regain good breathing:
Described below are breathing techniques to help you restore physiological balance and bring about relaxation. In essence, the general aim is to shift from upper chest breathing to abdominal and diaphragmatic breathing, create a calm inner state, and then to make good behavioural choices.
Abdominal breathing and the correct allocation of carbon dioxide directly connects to the parasympathetic arm (relaxation) of the autonomic nervous system and encourages inner calm and relaxation. The immune system is supported in moving away from a dominant inflammatory pattern to more inner balance. Other restored benefits such as good sleep, good nutrition and exercise help further. The ability to create a relaxation response helps people to feel more peaceful and perhaps find a spiritual connection. It only takes a quiet, relaxed environment where you won’t be disturbed for 10 to 20 minutes to tune breath and create good carbon dioxide levels.
Breathing Re-training: ‘Good breathing involves a three step process’:
Mechanical:
It is important for you to know how to engage the diaphragm and release old musculoskeletal holding patterns. Work with an Osteopath is often recommended. David worked with Jonathan whilst living in Cirencester and in Hampshire now works with Ashley Shah in his Alresford clinic.
For balanced breathing sit comfortably and feel your lower ribcage expanding as you breath in and your abdomen rising. Place one hand on your chest and the other on your abdomen. Notice how your upper chest and abdomen are moving while you breathe. Become aware of your breath and allow yourself to breathe in and out gently through the nose. Your upper chest movement will diminish as you use the diaphragm that is acting like a parachute opening out as you breathe in. This feels as if the ‘soft belly’ is expanding as your lower ribs move out. Because your diaphragm is attached to the upper lumbar vertebrae you may feel your back moving out as well as the muscle descends. You may find it easier to sense these movements lying on your back with your knees and neck supported. For those of you who show signs of chronic over breathing the process to recovery is longer and often requires more complex body work with a trained body worker, combined with capnography feedback and mindfulness approaches. Other skills such as the ‘body scan’ help restore and maintain sense perception so that the movements of the diaphragm can be sensed again and integrated into breath by breath awareness.
Volume Control:
Dysfunctional breathing pattern disorder or over breathing is a state in which the volume of air moved through the lungs during inspiration and expiration is too great for the metabolic requirements of the body. We use the phrase ‘less is more’ to get across that reducing the ‘tidal volume’ of air in and out increases carbon dioxide levels. It is often helpful to recognise the effects of changing breath volume by seeing the carbon dioxide responding directly using capnography. The expiratory phase of the breath is associated with the relaxation response so that teaching how to prolong the out breath with a whispered ‘ah’ sound or the Ujjay breathing taught by yoga practitioners is an important skill for you to learn. David has made a ‘breaking waves’ CD in which the sound of the breaking wave encourages a longer out breath.
Mindfulness: Changing Breath as a Behavioural Response:
Once you are happy with the technique it is important to practice changing breath responses in challenging situations. The AWARE response is a useful technique which can be practiced in response to an imagined stressor and then in the actual challenge situation, for example in panic attack disorder:
A = An Activating event
W = Watch rather than react
A = Notice your Anxiety or Body sensation response and reduce physiological arousal by:
R = Slowing your Respiration with the lengthening of the out breath where the ratio of the in to the out breath is 4:6 (silent count of) 4 in and (silent count of 6 out) and after the out breath the silent words of ‘changing over.
E = Bring in with the in breath a remembered sense of Enjoyment and self Empowerment.
Sustained stress and body-mind protest:
Each of us has a limit of tolerance to ‘stresses’ where we move away from the stress response that is appropriate to appropriate challenges. Too little challenge, as when on the lower ‘up slope’ of the stress curve ( see below) is also stressful. Too much pressure from the inner world of emotions or the external world of too much demand may overwhelm your perceived ability to respond with energy and focus. This then may lead you onto the ‘down slope’ when these challenges are too much. The sustained catabolic state mobilises defences and activates the limbic system of the body as well as releasing sugar, cholesterol and further disturb internal homeostasis – the catabolic metabolism. Body symptoms as well as ‘mental’ – mind body duality doesn’t exist - are a major challenge to health services where as many as 50% of those attending general practitioners have ‘medically unexplained and functional ill health.[13] Treatment with medication rather than explanations that connect to the individual’s life situation is often not helpful and very expensive. An educational model is likely to be the way forward.
Summary and Further Reading:
In this article we have endeavoured to convey the effects in your body resulting from sustained stress. Over breathing is often overlooked although increasing recommended as part of other therapies. In Cognitive Behavioural Therapy – Applying empirically supported Techniques[10] it states that ‘individuals with chronic anxiety symptoms such as panic attack disorder and generalized anxiety disorder are most likely to benefit from breathing re-training’ . Alicia Meuret and colleages have shown convincingly in panic attack disorder the value of capnography[14] and The textbook Multidisciplinary Approaches to Breathing Pattern Disorder[7] gives a fuller account of this subject.
The positive experiences of a skeptic using breath and mindfulness:
Tim Parks, quite separately from our work, describes eloquently his recovery from many years of chronic pain. He describes his journey in his book Teach Us to Sit Still: A sceptic’s search for health and healing.[15] He describes his own experience of combining breath work and mindfulness moving from a position of self professed cynic before he found improvements in his long standing unexplained chronic pain. His recovery was complete as he added meditation and mindfulness.
References:
1. Thich Naht Hahn The Miracle of Mindfulness Beacon Press 978-0-8070-1239-0. 1999.
2. Tolle Eckhart. Practising the Power of Now: Hodder Mobius 978-0-340-82253-1. 2001.
3. Segal V; Williams J; Teasdale J. Mindfulness Based Cognitive .J Van Dixhorn 1985 Journal of Psychological Research 29(2)199-206. 2002.
4. Behavioural Therapy for Depression Guilford ISBN 1-57230-706-4
5. Clive Cookson. Science April 23/24 FT.com. 2011.
6. Krapf and colleagues. Chronic Respiratory Alkalosis Vol 324; (20). 2001.
7. Chaitow L; Bradley D, Gilbert C. Multidisciplinary Approaches to Breathing Pattern Disorders Churchill Livingstone. 2002.
8. Giannattasio C, Failla M, Meles E, Gentile G, Grappiolo A and Mancia G. “Efficacy of self treatment of hypertension at home with device-guided breathing.” Am J Hypertension 2002; 15(4,2)186A. 2002
9. Van Dixhorn J; Journal of Psychological Research 29(2)199-206. 1985.
10. Cognitive Behavioural Therapy: Editor O’Donohue W. Applying Empirically Supported Techniques Wiley. 2008.
11. www.nice.org.uk/guidelines
12. Beales D; Whitten H Emotional Healing for Dummies – Wiley- 978-0-370-74764-3. 2010.
13. Beales D. Beyond Mind-Body Dualism: Implications for patient care Journal of Holistic Health Care 2004 1:3 15-22. 2004.
14. Meuret Alicia and Ritz T. Hyperventilation in panic disorder and asthma: Empirical evidence and clinical strategies – Department of Psychology, Southern Methodist University, Dallas. TX, 75206, USA. 2010.
15. Parks T. Teach Us to Sit Still: A Sceptic's Search for Health and Healing Harvill 978-1-86-55399-8. 2010.
16. Thomas, M and colleagues. Breathing retraining for dysfunctional breathing in asthma: a randomised controlled trial Thorax, 58 (2): 110-115. 2003.
Further Information
Hawkwood College: Mindfulness and Breath: Optimise your Health and Wellbeing
Tutors: Dr David Beales FRCP MRCGP Dip Psych and Jonathan Nunn DO
Date: Saturday, 30 Jul - Sunday, 31 Jul 2011.
Hawkwood College, Painswick Old Road, Stroud, Glos GL6 7QW. Tel: 01453 759034; www.hawkwoodcollege.co.uk www.hawkwoodcollege.co.uk/courses/Mindfulness_And_Breath_July
Booking Form: www.hawkwoodcollege.co.uk/booking/form.php
Comments:
-
No Article Comments available