Positive Health Online
Your Country

The Nasopharynx
listed in dentistry, originally published in issue 281 - September 2022
Originally published The Nasopharynx
The nasopharynx represents the most superior portion of the pharynx, bounded superiorly by the skull base and inferiorly by the soft palate. The nasopharynx connects the nasal cavity to the oropharynx and contains the Eustachian tube openings and adenoids on each side.
The Eustachian tube is amenable to harm from:
- Inadequate drainage.
- Infections
These problems emanate from:
- A poor swallowing pattern, for many reasons as shown in various parts of this forum. Briefly, when one swallows correctly the tongue descends at the back of the throat creating a vacuum which allows proper drainage of the nasopharyngeal tubes and keeps it healthy. In cases where patients have a poor developmental growth of their jaws and teeth, the tongue function goes wrong and when swallowing it rises posteriorly causing a positive pressure in the oropharynx which prevents the drainage of the tube giving rise to stagnation and infection.
- The excessive use of toothpaste and mouthwashes does not help. They kill the normal commensal bacteria necessary for good oral health causing resistant organisms to take hold in the throat. The main ones have been found to be bacterial Staphylococcus Aureus and Pseudomonas Aeruginosa dominant infections which create a biofilm.
If one gets infected with a viral infection these bacteria rapidly increase and one can get a serious nasopharyngeal tube infection apart from developing a sore throat.
The continued use of the toothpaste and mouthwashes which kill the commensal organisms giving rise to these secondary bacteria. These PREVENT ANY HEALING OF THE THROAT if a new infection manifests itself.
It is therefore of the utmost importance that one tries to prevent Staphylococcus Aureus and Pseudomonas Aeruginosa dominant biofilms from toothpaste and mouthwash use.
If you or your child wake up in the morning with a bad breath, then you know you suffer from such an infection.
To illustrate the point it would be interesting to read the experiences of one such person:
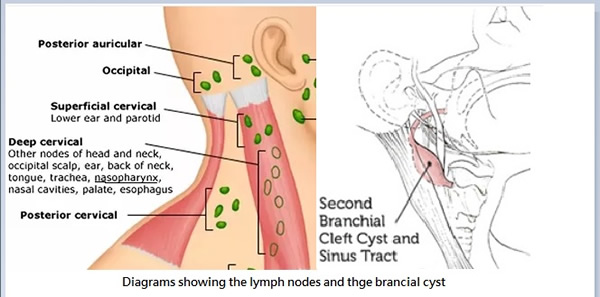
A patient turned up with a swelling on her neck. On palpation, it felt like a lymph node swelling. I looked up my diagram and it confirmed that this was more likely to be a superficial cervical lymph node.
An intra oral examination showed severe infection of the gingivae and a very sore throat. She complained of deafness on the left side which was the same side as the lymph node swelling. This raised a concern that probably her naso-pharyngeal tube was infected which had given rise to the cervical lymph node swelling. She was also suffering from a very high fever.
She had thick slimy saliva that coughing was unable to dislodge indicative of heavy use of toothpaste which often gives rise to resistant organisms as mentioned earlier. Her gingiva was very swollen and easily bled again confirming the use of toothpaste.
Her gingival condition had been discussed and treated on previous occasions. Despite warning her about the toothpaste she continued to use it.
Because of her high fever, I spent a few minutes clearing her gingivae and referred her to the local hospital for urgent intravenous antibiotic treatment. She was told that she had a branchial cyst on the neck which needed surgical attention and because "her infection was viral" no antibiotic was indicated. This, despite her very high fever.
Patients who have been researching covid might have looked up the 1920 Spanish flu investigations where recent examination had shown that Bacterial Pneumonia Caused Most Deaths in the 1918 Influenza Pandemic https://www.nih.gov/news-events/news-releases/bacterial-pneumonia-caused-most-deaths-1918-influenza-pandemic. The patients had actually died of bacterial NOT viral infection.
Please note all viral infections become severe bacterial infections within hours. Antiviral agents like Remdesivir cause kidney failure engorging the lungs with fluid with the rapid demise of the patients. Multi organ failure follows. (This has then been blamed on the sars cov 2 virus and not on the exclusive use of the antiviral as against the necessity to use an antibiotic.)
During the night my patient became very unwell and was taken by ambulance to a major teaching hospital in London where she was finally given intravenous antibiotic treatment and again informed that she had a branchial cyst which needed surgical removal.
I knew the family well and took along a very highly qualified medical doctor friend with me to see her in hospital. He agreed with me that it was indeed a lymph node swelling and not a branchial cyst.
After a couple of days with IV antibiotics, the cyst shrank a little and her fever also subsided. She was discharged to return in a month for the removal of the branchial cyst.
After this, she went back to Sweden where everything flared up again. She had not stopped the toothpaste.
Again, she was hospitalized, and told that she needed surgery to remove the branchial cyst. I reasoned with her that her throat is not going to recover with the removal of the supposed branchial cyst until she stops the toothpaste and uses saltwater instead.
She finally paid attention and gradually her gingivae, her throat, and the Eustachian tube all recovered. The lymph node swelling also disappeared (never to return again 3 years on). There never was a branchial cyst.
She was also trained with Myofunctional therapy to improve her swallowing pattern.
Branchial cysts do not disappear. A branchial cyst is a lump that develops in the neck or just below the collarbone. Branchial cysts form during the development of the embryo. They occur when tissues in the neck and collarbone area (branchial cleft) fail to develop normally.
If the medical doctors had looked at her condition in a holistic way noting the presence of partial deafness and a severe throat infection and fever they would have been able to differentiate it from a lymph node enlargement.
The improvement or benefits identified in the testimonials and articles on this site are based on individual experiences which are dependent upon the patient’s unique health condition, jaw condition, occlusal position, medical history, and other individualised factors, and should not be considered representative of all treatment outcomes.
Comments:
-
No Article Comments available