Positive Health Online
Your Country

Heart Failure or Therapy Failure? Toxins Cause Cardiomyopathy
listed in heart, originally published in issue 293 - March 2024
Originally published at: orthomolecular.activehosted.com
also at: tomlevymd.com
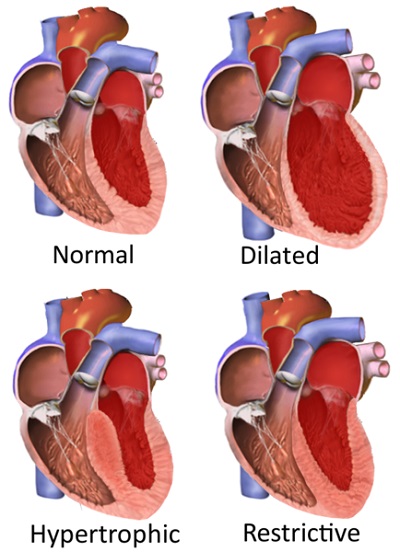
Cardiomyopathy simply means heart muscle disease. [1] It can occur as a primary affliction of the heart muscle, from a secondary condition negatively impacting heart function, or from a combination of both these clinical conditions. [2,3] Relatively recent changes in the definition of cardiomyopathy have been put forward that differ somewhat with these long-standing categorizations of heart disease. However, for the practicing clinician, the most important considerations in approaching the cardiomyopathy patient with clinical heart failure are:
- Is the heart muscle itself diseased?
- Is the heart muscle normal but being forced into failure by non-cardiac factors?
- Is the clinical presentation a combination of both these conditions?
- Is the treatment protocol aimed only at relieving symptoms or also at resolving the underlying pathology resulting in the clinical heart failure?
https://en.wikipedia.org/wiki/File:Tipet_e_kardiomiopative.png
Types of Cardiomyopathy
Credit: Npatchett, User:BruceBlaus via Wikipedia
Because cardiomyopathy presenting as clinical heart failure is a condition typically involving multiple factors, there is no single clinical protocol that can be considered the optimal treatment plan. Furthermore, heart failure rarely occurs by itself without other diseases and co-morbid conditions being present and contributing to symptoms as well. [4,5] However, all presentations of heart failure share features that should always be addressed clinically, regardless of whatever other treatments are being administered. The huge public health impact of heart failure cannot be overstated. In Germany, for example, heart failure is the most common primary inpatient diagnosis. [6]
Heart Failure Pathophysiology
When the function of the heart is impaired sufficiently to decrease the amount of blood that should be pumped with every heartbeat (cardiac output), a clinical picture of heart failure will eventually emerge. As the body can clinically compensate reasonably well for early heart failure, it is only when the decreased function is severe enough and chronic enough that heart failure symptoms become clear-cut. Because of this, even seemingly mild heart failure symptoms should be taken very seriously, with a complete diagnosis (especially in the ongoing pandemic setting), and the application of scientifically-based treatments for supporting and improving heart function.
Common symptoms of heart failure include the following, due basically to the abnormal accumulation of fluid in the lungs and the rest of the body from inadequate heart pumping ability: [7,8]
- Shortness of breath at rest or too quickly with exertion
- Shortness of breath when lying flat
- Waking up suddenly short of breath
- Fatigue
- Swelling in feet, ankles, and eventually legs and/or abdomen
- Accelerated heart rate, palpitations
Heart muscle cells do not just fail and "wear out" for no reason. When oxidative stress increases inside the heart tissue, inflammation by definition then exists as well. Also, part of that increased oxidative stress is the result of decreased ATP (adenosine triphosphate) production in the mitochondria of the heart cells. As ATP is the main energy-providing molecule in the body, those heart cells that have compromised ATP production have more oxidative stress, which results in a clinical picture of inflammation, or myocarditis.
When the factors increasing oxidative stress are intense and acute in onset, rapid heart enlargement with poor heart contraction (congestive cardiomyopathy) will result. However, when the factors increasing oxidative stress are less intense and more chronic in nature, the heart will generally first "adapt" by increasing the heart wall thickness without enlargement of the left ventricular dimensions (hypertrophic cardiomyopathy). A clinical picture of heart failure will still be present and continue to evolve as the heart wall thickening makes the left ventricle stiffer and less compliant. This results in that heart chamber not filling up as readily (diastolic heart failure, or heart failure with preserved ejection fraction). [9,10] Effectively, this form of cardiomyopathy actually consumes more ATP trying to fill the heart than to empty it. [11]
With this resistance to chamber filling, the amount of blood pumped with each heartbeat decreases while the blood supply coming into that chamber "backs up," resulting in the heart failure symptoms noted above. To be discussed below, toxins cause both forms of cardiomyopathy. Left untreated, the terminal stages of hypertrophic cardiomyopathy evolve into a congestive cardiomyopathy, with substantial enlargement of the left ventricle and very poor contractility. This will result even when the heart was not enlarged or poorly contracting at the onset of the myocardial inflammation. The initial clinical presentation of heart failure is roughly split equally between hypertrophic and congestive cardiomyopathy. [12]
Limited blood flow in the heart (ischemia) is commonly considered to be the cause of congestive cardiomyopathy most of the time. This is certainly a major reason for heart failure when multiple heart attacks with death of heart muscle and fibrotic scarring are present in place of contracting heart muscle. However, heart biopsies in consecutive patients with advanced coronary artery blockages and clinical heart failure indicated otherwise. The microscopic evaluation of these biopsies indicated that myocarditis was the underlying cause, and heart function in some of these patients improved dramatically with anti-inflammatory measures. In the absence of active ischemia or old heart attacks with extensive loss of heart tissue, it is erroneous to consider ischemia as a primary cause of congestive heart failure. The important takeaway point is that myocarditis is not necessarily an obvious diagnosis. There must be a lower threshold for taking heart tissue biopsies, as missing the diagnosis of a treatable condition greatly increases morbidity and mortality for many patients. [13]
Toxins and the Heart
While toxin accumulation in the heart muscle can be the singular cause of advanced heart failure, it will much more often be one of several factors contributing to decreased heart contractility. Also, the chronicity of the heart failure, regardless of cause, will play a large role in determining its reversibility, as more and more inflamed heart cells will eventually die and not just remain in a chronically inflamed state. Such inflammation is consistently seen on the microscopic study of heart biopsies in toxin- and infection-related cardiomyopathy. [14,15] Many different toxins, including many heavy metals, have been either linked to heart failure or clearly shown to be the direct cause. Furthermore, one or more of these toxins is nearly always present in high concentrations in the affected heart muscle. A partial list of such agents includes the following:
- Lead
- Copper
- Iron
- Mercury
- Aluminum
- Cobalt/Chromium
- Cadmium
- Gold/Silver
- Chemotherapy
- COVID Spike protein
Lead: In a 3-year-old girl with chronic lead poisoning, acute heart failure developed that was clinically reversed after four days of calcium EDTA chelation therapy. [16] Children who died from heart failure secondary to acute lead poisoning were documented to have the microscopic findings of myocarditis. [17] Lead has been shown in other studies to target the heart and the vascular system. [18-21] Animal studies have also shown that enough lead exposure will reliably cause myocarditis and vascular damage as is seen in humans. These studies show that lead exposure will cause atherosclerosis and high blood pressure as well. [22-24]
Copper: A transition metal necessary for normal cell function but easily pushed to excess and toxic levels in the body, copper is another culprit toxin commonly involved in cardiomyopathy patients. [25,26] Excess copper appears to be especially toxic to the heart, as the infusion of copper into the coronary circulation of rats results in impaired heart function in only minutes. [27] Hypertrophic cardiomyopathy has been strongly linked to the excess copper levels seen in Wilson's disease. Trientine, a selective chelator of copper, has been shown to improve cardiac function in hypertrophic cardiomyopathy patients. [28]
In a randomized, placebo-controlled trial on diabetic patients with left ventricular thickening (that can lead to hypertrophic cardiomyopathy), copper chelation significantly decreased the heart wall thickening. This study did not even screen for elevated copper levels. [29,30] Furthermore, trientine chelation in diabetic rats with advanced left ventricular failure over an eight-week period demonstrated significantly improved heart function. [31] Another heavy metal-removal study in diabetic rats with either trientine or citrate (citric acid) significantly protected heart function. [32] In a case report a patient with scleroderma and a congestive cardiomyopathy improved dramatically on penicillamine, an effective chelator of copper, lead, and mercury. No copper level testing was reported as part of the evaluation of this patient. [33] These studies further indicate that toxicity from copper and/or other heavy metals in the heart is often a significant contributing factor in patients with early heart wall thickening and then its later decompensation into decreased cardiac function and heart failure.
It appears that a clear diagnosis of copper excess does not need to be made before just treating patients presumptively as having too much copper in their heart, especially when heart wall thickening is present in a diabetic patient. [34] It has also been shown a copper-overload state is a primary factor in the pathogenesis of damage to any organ in the diabetic. [35] Copper removal has also been shown to decrease the inflammatory response to radiofrequency ablation treatment for liver cancer in rats. [36] These findings strongly suggest that:
The unsuspected presence of excess copper in tissues and organs can impair the resolution of ANY pathology being treated, indicating a positive role for copper removal for nearly all medical conditions.
Iron: Congestive heart failure secondary to severe iron overload in the body has been described. The daily administration of an iron chelator (deferoxamine) in a congestive cardiomyopathy patient over roughly a year dramatically improved heart function and cardiac output, with heart pumping ability more than doubling (ejection fraction from 20% to 48%). [37] Another case report described a 27-year-old woman with "severe heart failure" completely normalizing on an iron removal regimen. [38] Patients with severe iron overload cardiomyopathy have an average survival of only one year when therapeutic phlebotomy (blood donation) and iron chelation are not utilized. This form of cardiomyopathy begins with restricted filling of the heart (diastolic dysfunction), and then evolving into a congestive cardiomyopathy. [39]
Iron overload cardiomyopathy occurs most commonly in patients with hereditary hemochromatosis or secondary hemochromatosis (as with β-thalassemia and sickle cell anemia). [40] However, excess iron short of that seen in full-blown hemochromatosis can still be expected to inflict its own dose-dependent toxicity. Most adults already have excess levels of iron in their bodies, as reflected by elevated ferritin levels that erroneously remain regarded as normal in laboratory reference ranges. [25] Excess iron in the heart is also a predisposing factor to developing atrial fibrillation, an arrhythmia that contributes its own increased morbidity and mortality. [41]
In animal studies, excess cellular iron in heart cells has been shown to increase oxidative stress and impair the ability of the mitochondrial electron transport chain (ETC) to produce ATP. As ATP is the primary energy-providing molecule in the body, any decrease in its production always results in compromised cellular function and disease. [42,43] Of note, resveratrol supplementation has been shown to dramatically improve heart function in animal models of iron overload cardiomyopathy. [44-46] In another animal study, either deferiprone or N-acetylcysteine was effective in decreasing cardiac iron concentration. [47]
Mercury: As the most toxic non-radioactive element, mercury is a heavy metal that causes grave damage wherever it accumulates. A landmark study directly compared toxic heavy metal concentrations in biopsies of heart muscle against control muscle biopsies in patients with idiopathic dilated cardiomyopathy (IDCM), meaning advanced heart failure of unknown cause. The cardiomyopathy heart muscle had 22,000 times more mercury in it than in normal heart muscle. Versus normal specimens, the same diseased heart muscle had 12,000 times more antimony, 11 times more gold, 13 times more chromium and 4 times more cobalt. Of great significance, there was no primary screening to detect increased heavy metal exposure in the study group, meaning these accumulations likely represent the finding in most cases of IDCM. [48] Unless excess exposures to heavy metals are readily apparent, the widespread effects of such poisonings make it very unlikely that such a toxicity will be suspected and then correctly diagnosed. [49]
In another study, the heart muscle in cardiomyopathy patients examined at autopsy revealed significantly higher levels of lead, nickel, copper, and manganese, and significantly lower levels of zinc compared to the heart muscle in non-cardiomyopathy patients. Mercury and antimony levels were not reported and presumably had not been measured. [50] This study indicates that most patients with IDCM have not only astronomical levels of mercury and antimony, but also significant elevations of lead, nickel, and copper. If it was not a vital organ, the ability of the heart to selectively remove heavy metals out of the blood and the rest of the body could be considered a protective mechanism for the health of the body! This leads to the conclusion that:
Cardiac muscle in patients with advanced congestive cardiomyopathy is the preferred collection site for most of the heavy metals taken into the body.
Currently, IDCM is the cause of heart failure in over 100,000 people in the United States, and it is the underlying diagnosis leading to 45% of heart transplants. Furthermore, evidence of resolved or ongoing viral infection in heart biopsy specimens are seen in 25% of IDCM patients. [51] Up to 80% of IDCM patients demonstrate one or more anti-heart autoantibodies. [52] Such antibodies are commonly the result of occult infections. Heavy metal accumulations and chronic viral myocarditis appear to be pathology-precipitating partners. [53] While it is unclear whether one factor better facilitates the presence of the other, it appears that heavy metal accumulation, headed by mercury, is a very common cause of IDCM. Based on these studies that have specifically measured heavy metal status in IDCM heart muscle, heavy metal accumulation appears to be the culprit for this advanced form of heart failure MOST of the time. The IDCM heart would appear to be a chemically attractive site for the accumulation of multiple heavy metals after being primed by an earlier myocarditis-precipitating viral infection, as no other organ in the bodies of IDCM patients appears to similarly concentrate these toxins.
Mercury also works effectively to produce a deficiency state of selenium. Restoring deficient selenium stores can lessen clinical mercury toxicity, although it does not directly promote the mobilization or elimination of mercury. Congestive cardiomyopathy secondary to selenium deficiency has been reported, and restoring depleted selenium levels can reverse it. [54-57] Based on the data above on mercury and IDCM, a cardiomyopathy associated with selenium deficiency is likely a cardiomyopathy due to the toxicity of excess mercury no longer being negated by a sufficient presence of selenium. Of note, too much supplemental selenium has its own toxicity, unlike many other nutrient supplements, and should not be overdone.
Aluminium: Aluminium phosphide, an agent used as a pesticide, induced a severe, but reversible, cardiomyopathy after accidental poisoning in an exterminator. [58] Intense supportive care to reverse low blood pressure was shown to facilitate the recovery of other individuals poisoned with aluminum phosphide that resulted in severe compromise of heart contractility. [59,60] In a hemodialysis patient who expired with heart failure, heavy aluminum deposits were seen in the heart cells upon electron microscope examination. [61] An animal study also showed that aluminum chloride could induce a largely reversible cardiomyopathy. [62] Organic acids (succinic, malic, or citric) and the iron chelator, desferrioxamine, are agents that can mobilize (solubilize) and eliminate aluminum accumulations. [63]
Cobalt/Chromium: Cobalt is another toxic heavy metal documented as a cause of congestive cardiomyopathy. Elevated blood cobalt levels have been identified in some metal hip implant patients. [64,65] Elevated blood chromium levels from the implants can be seen as well. [66,67] However, the presence of such elevations is not an assurance that a cardiomyopathy will result. [68] As noted above, IDCM often starts with an undiagnosed viral myocarditis. Such a myocarditis would appear to inflict the myocardial damage that triggers the almost sponge-like uptake of cobalt and other heavy metals, as described in the section on mercury accumulation in the heart. An animal study also showed that poor diet (protein restriction) further predisposed the heart to cobalt toxicity. [69] N-acetylcysteine is effective in significantly reducing the blood concentrations of both cobalt and chromium. [70] Alpha lipoic acid is another effective chelator of cobalt. [71]
Cadmium: A study examining blood, serum, and urine heavy metal levels found significantly higher cadmium levels in IDCM patients than in healthy controls. [72]
Gold/Silver: While gold and silver are not recognized as toxic substances in general, some care always needs to be exerted in a supplementation regimen, especially one involving metals. In a case report, a dilated congestive cardiomyopathy resulted from the excessive ingestion of colloidal gold for about three months, along with a history of intermittent colloidal silver ingestion over the prior seven years. In addition to an enlarged heart that was contracting poorly, a significant new heart conduction abnormality (left bundle branch block) resulted from this supplementation. Following chelation therapy (dimercaprol) the block disappeared and the ejection fraction of the heart improved from 20% to 50%, a very dramatic improvement. Of note, urine screening (no tissue levels measured) revealed no evidence of excess aluminum, arsenic, barium, beryllium, cadmium, copper, manganese, or thallium. [73]
Chemotherapy: Cancer chemotherapy utilizes some agents that are highly toxic to the heart. Anthracyclines (doxorubicin, idarubicin, epirubicin, mitoxantrone) often result in some heart enlargement and decreased contractility. [74,75] These are cardiac effects that are still considered to be largely irreversible, even though chelation therapy has been shown to be effective in preventing such cardiac damage. [76-79] Considering that multiple toxins and heavy metals are typically present in patients with IDCM, it should not be assumed that trying to remove as much of the toxin load from the body (and the heart) will be of no benefit. Cancer patients typically have other diseases as well, and it is reasonable to think that some of these patients (such as those with the copper accumulation often seen in diabetes) might have already been accumulating cardiac toxins before there was any evidence of cardiac compromise. As such, chelation therapy would have the potential to at least partially reverse the cardiac damage currently seen with chemotherapy.
COVID Spike Protein: Persistent spike protein (PSP) syndrome is seen when the COVID pathogen-related spike protein stays in the body following a COVID vaccination and/or because it was never completely eliminated following an unresolved COVID infection (chronic or long-haul COVID). [80-82] While the spike protein has been found throughout the body in autopsy studies on COVID patients, it appears to have a particular predilection for attacking the heart and its blood vessels. [83-88]
The spike protein inflicts damage in the heart and elsewhere in the body by multiple mechanisms. These mechanisms include:
- Facilitating COVID pathogen entry into cells (ACE2 receptor binding). [89-91]
- Overstimulation of the immune response by being chronically present, evolving into an autoimmune disease. [92-94]
- Attacking not only tissue and organ cells directly, but also the walls of the blood vessels and the platelets circulating in them, resulting in the increased formation of blood clots. [95,96]
- Intrinsic toxicity of both the complete spike protein as well as fragments of it. [97-99]
- The ability to enter the genome of the cell where it currently cannot reliably be eradicated, along with the seeming ability to be replicated indefinitely. [100]
Myocarditis, often evolving heart enlargement and heart failure, can result from the spike protein exposure following COVID vaccine(s) and/or from its persistence presence in chronic COVID. However, many cases of spike protein myocarditis, probably a substantial majority, are chronic, smoldering conditions that remain undiagnosed except when there is clear clinical evidence indicating its presence.
PSP syndrome routinely involves the heart, even when not readily apparent clinically. In fact, the spike protein has such a preference for heart muscle that chronic COVID or post-vaccination patients are unlikely to ever have spike protein or its pathological impact elsewhere in the body while sparing the heart. In autopsies of patients who died of COVID-19, either COVID-related viral RNA or evidence of myocardial inflammation was seen more than 80% of the time. [101] Another autopsy study revealed spike protein presence over 60% of the time. [102]
Clinically significant myocarditis secondary to PSP can often be missed and completely unsuspected clinically due to the patchy and limited nature of many cases of spike protein myocarditis. [103] In a case report, conduction system cells (AV node) of the heart were selectively inflamed, suggesting why even a minimal, undetected spike protein myocarditis can trigger lethal arrhythmias. [104] In another case report autopsy, the spike protein in the heart was most dominant in the AV node as well as in the pacemaker cells in the atrium. Scattered throughout the heart were single necrotic (dead) heart cells, adjacent to viable cells. [105] Another autopsy study also reported this single-cell death in COVID hearts. [106,107]
Unlike the other toxic cardiomyopathies, spike protein only rarely involves the whole heart, and the amount of heart muscle involvement can be very minimal. Nevertheless, sudden cardiac death (not from a heart attack due to "traditional" coronary atherosclerosis) is no longer uncommon, and it appears a substantial number of individuals around the world can be symptom-free and still be liable to life-threatening arrhythmias under conditions of stress, including previously-healthy young athletes. [108]
As the number of people with undetected spike protein/COVID myocarditis is enormous already and steadily increasing, part of the therapy for anyone felt to have persistent spike protein should still involve the regular administration of one or more heavy metal chelation agents. As discussed above, heavy metals appear to "await" the microenvironment of myocardial inflammation of a previous viral infection to begin accumulating, if they have not already accumulated there prior to the COVID infection or the vaccine administration. As with all other toxins, heavy metals will always substantially worsen any inflammation and electrical instability already caused by the presence of the spike protein and the COVID pathogen. Most likely this worsening is synergistic in nature, and not just the additive effect of spike protein and heavy metals.
Before the diagnosis of idiopathic (unknown origin) cardiomyopathy is made, toxic and infectious causes must be ruled out. If the absence of these causes is not clearly established, prophylactic nutrient chelation should always be part of any therapeutic protocol, or the reversibility of clinical heart failure will never be realized. Currently, such diagnostic effects are rarely made. [109]
ATP Physiology and Cardiomyopathy
No cell, whether in the heart or elsewhere, is healthy when mitochondrial function and ATP production are chronically suppressed. Such suppression will reliably occur when the reduction-oxidation balance inside the cells is sufficiently shifted toward excess oxidation. All diseased cells have too little antioxidant presence, and this is reflected in higher cellular levels of calcium and lower cellular levels of magnesium, vitamin C, and glutathione. When these levels remain abnormal, mitochondrial ATP production will always be depressed as well. These cellular abnormalities are always present in diseased tissues or organs. [110,111]
When cardiac ATP production can be restored to optimal levels with a normal increase capability for exercise, a healthy heart will result, unless irreversible damage has already taken place. [112] Of note, mitochondria are especially abundant in heart tissue, and more than 90% of the energy of the heart is generated by these mitochondria. As the heart completely renews its ATP content every 20 seconds or so, it can demonstrate clear mitochondrial insufficiency (heart failure) when other organs appear to be less affected or completely unaffected. [113,114] No organ consumes more energy per gram of tissue than the heart. [115]
As the mitochondria are the intracellular sites of ATP (energy) production, significant research has been directed at finding ways to reverse or lessen "mitochondrial dysfunction." [116] Most cases of mitochondrial dysfunction are due to the increased oxidative stress resulting from chronic infection and toxin accumulation, although rare genetic defects in mitochondrial function can result in the same clinical pictures of decreased energy production. [117]
Much of this mitochondrial research has focused on defects in the electron transport chain (ETC) embedded in the membranes of the mitochondria. The ETC directly fuels the ATP synthase enzyme vital to the production of ATP at the end of that chain. The ETC has four main complexes, or steps, that work to optimally shuttle electrons to the terminal ATP-producing enzyme. [118,119] These complexes and their significant characteristics can be summarized and simplified as follows:
- Complex I: NAD (nicotinamide adenine dinucleotide) in its reduced form, NADH, starts the electron donation sequence.
- Complex II: FAD (flavin adenine dinucleotide) in its reduced form, FADH2, continues the electron relay to ubiquinone (oxidized coenzyme Q10 [CoQ10]).
- Complex III: Ubiquinol (reduced CoQ10) relays the electrons to cytochrome c.
- Complex IV: Cytochrome c oxidase then receives the electrons where molecular oxygen is bound and reduced to water.
- ATP synthase (also known as complex V) is then activated to complete the ETC electron shuttling with the subsequent production of ATP.
Mitochondrial dysfunction is most successfully addressed when the substrates of the ETC (NAD, FAD, CoQ10) are either directly supplemented or the precursors needed for their synthesis are supplemented. Fueling the ETC not only produces more ATP, it also results in less oxidative stress being generated in the process by the ETC agents as mitochondrial function becomes more efficient and total cellular oxidation declines. [120,121] And when ATP can be increased and oxidative stress can be decreased, mitochondrial healing can take place. Such healing is suggested in a study that found cardiovascular mortality to remain reduced for eight years following the completion of a four-year period of supplementation with CoQ10 and selenium. [122]
Defects in the ETC have been specifically identified in heart failure and are always present. [123] In even the most advanced cases of heart failure, most affected hearts still have inflamed but viable heart cells that can be positively impacted with improved ATP production. Aside from the chelation therapies noted above, bolstering mitochondrial function has been a major physiological goal in the treatment of heart failure. [124] While heart disease can occur from inherited mitochondrial disorders, most cases of heart failure are due to diseased mitochondria because of the pathogens and accumulated toxins in the heart. [125]
Traditional medicine has no drugs which directly work to normalize mitochondrial dysfunction in heart failure patients. Instead, all the current prescription drugs work only to basically mobilize excess fluid accumulations and/or to lessen the workload (peripheral resistance) faced by the failing heart muscle. This is not to say that there is no place for these drugs, only that they should not be the only agents given to the patient. As with most prescription drugs, the therapeutic goal appears limited to symptom improvement while letting the underlying pathology continue to evolve. Traditional medicine is much better at diagnosing and naming medical conditions than at reversing or resolving them.
When targeted therapies capable of entering the ETC of the mitochondria and improving ATP production are utilized, the clinical response in heart failure is often dramatic. These include many of the patients considered to have terminal congestive cardiomyopathies and no possibility of improvement or significant long-term survival without heart transplantation.
CoQ10 is the most researched of these ETC-targeted therapies for cardiomyopathy, and its enormous benefits on cardiac function have been well-documented. The especially vital role of CoQ10 in supporting ATP production in the heart is reflected in its concentrations in different tissues in the body. Far more CoQ10 is found in the heart than is found in any of 12 other human tissues examined. Furthermore, the heart contained roughly twice as much CoQ10 as the kidneys, the organ/tissue in the study with the second highest CoQ10 concentrations. Non-cardiac muscle had only one-third of the CoQ10 as the heart muscle. [126]
CoQ10 directly promotes the mitochondrial ETC by supporting the electron transfer in complexes I and II, as well as by its established role in complex III. Its impact in restoring heart function in cardiomyopathy has been significant and sometimes stunning, especially since this is a condition that is only given supportive care by traditional cardiologists while steady cardiac deterioration continues.
In a randomized, double-blind trial in 420 patients with severe heart failure and followed for two years, there was a 42% reduction in all-cause mortality and cardiac mortality in patients given 100 mg of CoQ10 three times daily. Fewer hospitalizations for heart failure occurred in the treated group as well. [127] The supplementation of selenium along with CoQ10 appears to be especially effective in reducing mortality in cardiomyopathy patients. [128]
The ejection fraction (EF), a measure of how effectively the heart contracts and empties on each beat, is the most direct objective and readily measurable parameter to evaluate cardiac function. EFs considered to be normal run roughly from 65 to 80%. EFs of 10% to 15% represent the greatest loss of cardiac function and are characteristic numbers for patients on heart transplant waiting lists. CoQ10 supplementation has rescued many patients considered to have terminal heart failure, and this has been accompanied by dramatic improvements in EF and functional capacity in most patients, with one study showing the mean EF going from 25 to 42%. [129-134] It should also be noted that increasing an EF from 15% to 25% can take a patient who has difficulty walking across the room without shortness of breath to one who can function normally as long as major physical stresses are avoided.
The initial pathology seen in the heart failure of hypertrophic cardiomyopathy with preserved EFs is also clearly improved with CoQ10 supplementation. [135,136]
Low CoQ10 levels, along with increased CRP (C-reactive protein, a marker of oxidative stress) levels have been documented in heart failure, whether due to coronary disease or of unknown cause. [137] Other studies have also shown that lower CoQ10 serum levels correlated with increased all-cause mortality in general, as well as in heart failure patients. [138,139]
Conversely, CoQ10 supplementation has been shown to decrease all-cause mortality in all subjects. Furthermore, the CoQ10 supplementation clearly increased exercise capacity in the heart failure patients while having no significant adverse effects or safety issues. [140-143] First discovered in 1955, the benefits of CoQ10 in heart failure have been documented extensively in the scientific literature for 50 years now, yet the established textbooks of medicine and medical therapeutic manuals make no mention at all about this vital nutrient antioxidant, much less its impact on congestive heart failure. [144-148]
As CoQ10 increases the energy production in all the cells in the body, it should not be surprising that studies have shown its benefits in a wide variety of diseases. Low levels have been documented in many medical conditions, along with evidence of its clear benefits when properly supplemented or administered. Such conditions include the following:
- Brain disorders, including Parkinson's disease and Alzheimer's disease, stroke, and depression [149-152]
- Autism [153]
- ADHD (Attention Deficit Hyperactivity Disorder) [154]
- Hypertension (high blood pressure) [155-158]
- Coronary artery disease (atherosclerosis) and acute myocardial infarction [159-162]
- Improved clinical outcome post-coronary bypass and post-coronary angioplasty [163,164]
- Atrial fibrillation [165]
- Asthma [166,167]
- Obesity [168]
- Fibromyalgia [169]
- Diabetes (improved glucose and lipid profile) [170]
- Multiorgan failure when genetically deficient [171]
- Improvement in chronic kidney disease [172]
- Chronic lung disease [173]
- Fatty liver disease [174]
- Chronically increased oxidative stress [175]
- Vertigo [176]
- Sepsis and any critical illness [177-179]
- Statin cardiomyopathy [180]
- Statin myopathy (skeletal) [181]
- Eye disease [182]
As CoQ10 is one of few vital antioxidants that is synthesized in the body, ageing accounts for much of its deficiency in the body. Older people make less CoQ10, generally have less of it in their diet, and have other medical conditions excessively consuming it. The average 80-year-old has only about 50% of the cardiac CoQ10 content as the average 20-year-old. [183,184] But its importance in cardiac function is the same regardless of age. Just as deficient hormone levels need to be restored to optimize health in the aging patient, CoQ10 needs to be similarly addressed as well, as it is essential for the optimal health of all cells. [185]
Additional supplementation can specifically target complexes I, II, and IV in the mitochondrial ETC to help optimize ATP production. Not only will such supplementation be of benefit in all the cells of the body, the increased ATP demands of the heart make them especially suited to help support and improve the failing heart. [186]
NAD (nicotinamide adenine dinucleotide) is the primary substrate fueling complex I. The primary way to keep NAD levels high, in addition to directly supplementing NAD itself, is to take large amounts of its primary precursor for being synthesized in the body. This role is served by niacin (vitamin B3) and its vitamers (like niacinamide). [199] Levels of both NAD and ATP have been documented to be significantly depressed in cardiomyopathy biopsy specimens. [187] Like CoQ10, niacin significantly improves all cardiovascular conditions, not just cardiomyopathy. [188-198]
A severe niacin deficiency state has also been documented to be the root pathology in schizophrenia and other brain disorders, consistent with the high ATP requirements of the central nervous system for normal function. [199] Severe niacin deficiency results in pellagra, a life-threatening condition that is also associated with diminished heart contractility. [200-202]
Riboflavin (vitamin B2) also plays a critical role in optimizing mitochondrial ATP production. It serves as a precursor, or building block, for FAD, the primary electron-transferring substrate in complex II of the ETC. [203] An animal study demonstrated that riboflavin can alleviate heart failure and improve cardiac metabolism. [204] It can also lessen the amount of damage that reduced blood flow, or ischemia, will inflict on the heart. [205] A genetic deficiency of complex II results in an advanced congestive cardiomyopathy, indicating its importance in this condition. [206] When FAD is targeted as an antigen by anti-mitochondrial antibodies, a dilated cardiomyopathy results as well. [207]
Complex IV of the ETC, involving the transfer of electrons via cytochrome c oxidase to oxygen, the terminal electron acceptor, is supported strongly by methylene blue (MB). [208] MB is a powerful redox dye that has been shown to benefit neurodegenerative diseases by increasing mitochondrial energy production. [209-212] Promoting ETC ATP production by directly supporting complex IV is especially significant since the oxidative stress generated in the first three complexes is avoided. This means that less net oxidative stress in generated in the cell without compromising ATP production, a rarely achieved therapeutic goal. [213] This effect is also why MB has been promoted as an anti-aging agent, as cumulative oxidative stress is the reason for all aspects of aging. [214] In cellular studies, MB clearly delays the process of aging. [215]
Consistent with its documented brain benefits, MB has also been shown to protect and heal the heart. Well-documented to completely rescue and cure patients with advanced treatment-refractory septic shock as a monotherapy, MB was also able to improve cardiac function in a septic shock patient who already had an advanced cardiomyopathy. [216-218] Other studies have confirmed this consistently positive effect of MB for septic shock. [219,220] Advanced states of hemodynamic shock without sepsis have also been resolved by MB treatment. [221] In animal studies, MB not only improves ETC energy production, it also decreases oxidative stress and improves NAD levels in the mitochondria. [222,223]
Cardiomyopathy Treatment
The proper treatment of any form of cardiomyopathy, but especially advanced congestive heart failure due to an enlarged and poorly contracting heart, needs to be directed primarily at:
- Toxin elimination
- Restoring normal cellular energy production
Toxin Elimination: A thorough diagnostic work-up is always optimal, although currently unlikely to occur as endomyocardial biopsy is rarely done, except to monitor for microscopic evidence of organ rejection following a heart transplant. And when it is performed, the measurement of heavy metal content is never a routine part of the examination. A provoked urine challenge test with an established chelation agent such as EDTA (ethylenediaminetetraacetic acid), DMSA (dimercaptosuccinic acid) or DMPS (dimercaptopropanesulfonate) often results in a significant release of multiple heavy metals, and it should be routinely be part of a cardiac failure workup. [224]
Mercury is detected in most people although it is often given little regard because no "obvious" mercury exposures are evident. However, the number of people exposed for many years to outgassing mercury amalgam dental fillings is enormous, and the astronomical levels of mercury found in many IDCM patients are nearly always secondary to these fillings. [225-228] Furthermore, a brisk release of mercury on urine chelation challenge should never be disregarded as inconsequential.
Hair analysis can also be very useful in evaluating heavy metal content in the body and should be done along with the provoked urine challenge. For example, autistic children had significantly higher levels of mercury, lead, arsenic, antimony, and cadmium compared to controls. [229] In another study, DMSA was shown to be effective in increasing mercury and antimony excretion in children with autism spectrum disorders. [230]
Heavy metal chelation is still rarely done, although it should logically become part of the standard-of-care treatment protocols for most medical conditions and diseases, even in the absence testing for heavy metal accumulation.
Antimony bears some additional attention, as its levels inside IDCM hearts were stunningly elevated as well. [48] Generally given little attention, antimony is as toxic, or even more toxic, than arsenic. [231] Finding IDCM heart muscle with 22,000 times the normal level of mercury and 12,000 times the normal levels of antimony must not be disregarded as a curiosity, but must be regarded as the major reason for the decreased heart function, and treated with that in mind. Significant antimony exposure is difficult to avoid, as levels in the air and water continue to increase due to multiple sources, including the significant leaching of antimony from plastic containers. [232-235]
Until definitively established otherwise, an enlarged and poorly-contracting heart (advanced congestive cardiomyopathy) must be assumed to be secondary to mercury and antimony accumulation in the heart muscle.
As discussed at length above, the evidence indicates that cardiomyopathies can been assumed to have significant heavy metal accumulation and/or ongoing low-grade chronic inflammation. Also, toxin presence in the form of spike protein accumulation will be encountered with increasing frequency in this continuing COVID pandemic.
Regardless of any test results, all cardiomyopathy patients should be taking one or more chelating, or toxin-mobilizing, agents. Furthermore, follow-up blood, urine, and/or hair testing should be done to establish that toxins are being mobilized because of the chelator administration. When testing clearly indicates high levels of one or more heavy metals in the heart, potent prescription chelation administration is often advisable, especially when heart failure is advanced. Such agents include, but are not limited to, the following: [236]
- EDTA (orally, intravenously; calcium disodium EDTA best choice)
- DMSA (orally; especially good for mercury and antimony) [237,238]
- DMPS (intravenously-very potent, can cause substantial detox symptoms)
- Dimercaprol (British anti-Lewisite [BAL]) [239]
- Penicillamine
- Deferoxamine
- Trientine (especially copper)
Important nutrient chelators or toxin mobilizers:
- Organic acids, including alpha lipoic acid, citric acid, and ascorbic acid [240-243]
- NAC (N-acetylcysteine)
- Glycine
- IP6 (inositol hexaphosphate)
- Carnitine [244]
- As much of a wide variety of antioxidants as is feasible, including bioflavonoids, amino acids, and any supplement or food with a high organosulfur content. [245] Most chelators, including the prescription agents, are synthetic amino acid derivatives . [246]
Cellular Energy Production: All cardiomyopathies have deficient to severely deficient mitochondrial production of ATP. While a broad spectrum of quality supplements is always beneficial for any disease or medical condition, specific supplementation with a sufficient dosage is required to optimize ATP production in the cells of the heart. A suggested regimen of supplementation to achieve this goal would be as follows:
- Vitamin C as ascorbic acid or sodium ascorbate, three to nine grams daily
- Magnesium, any of multiple forms, one to three grams daily
- Vitamin D3, 3,000 to 10,000 units daily, with a blood level target of 50 to 100 ng/cc
These three supplements are essential baseline supplements, as each one works to lower intracellular calcium levels, decrease oxidative stress in all cells, and to decrease all-cause mortality. [247-252]
Supplements to stimulate and support mitochondrial ATP production:
- Niacinamide, one to three grams daily (or NAD supplementation)
- Riboflavin, 200 to 400 mg daily
- Coenzyme Q10 (ubiquinone or ubiquinol), 300 to 900 mg daily
- Methylene blue, 10 to 25 mg daily
The seven supplements above should be taken by all cardiomyopathy patients. As ATP is important in all cells of the body, these seven supplements can also produce significant clinical benefits in nearly all other medical conditions as well. The following nutrient supplements also support mitochondrial ATP production and can be added to the overall chelation/supplementation protocol as desired:
- Tyrosine (a CoQ10 precursor)
- Selenium (often depleted in cardiomyopathy)
- Succinate [253]
- 5-aminolevulinic acid (supports cytochrome c oxidase function) [254]
- Glycine (helps produce 5-aminolevulinic acid) [255]
- Ribose (rate-limiting precursor for adenine nucleotide synthesis and ATP production) [256]
- Carnitine (increases ATP; its deficiency also induces cardiomyopathy) [257,258]
- All dosing of prescription and supplemental agents should be under the guidance of the healthcare practitioner managing the care of the patient. The above agents are intended to be a general guide only. Clinical response and serial changes in laboratory testing are the main ways to determine how well a given patient is responding.
Recap
The heart muscle in all cardiomyopathies is depleted in ATP, the most important energy-producing molecule in the body. The worse the cardiomyopathy, the more severe the depletion. Nearly all the time, this ATP-depleted state is precipitated and maintained by heavy metal accumulations, often accelerated by earlier pathogen-provoked myocardial inflammation (myocarditis). Such myocarditis is typically undetectable on routine chemistries, and only more invasive testing can clearly document it.
When a patient presents with an enlarged, poorly contracting heart, it must be assumed that significant heavy metal accumulations are present and the treatment protocol must include chelation/toxin mobilization therapy.
Depending on the patient history and laboratory findings, the clinician needs to decide whether chronic COVID with low-grade spike protein-mediated inflammation is a major (or entire) part of the pathology involved. If this is confirmed, or if clinical suspicions are high, measures to eradicate the spike protein should be vigorously pursued. [80-83]
In addition to the heavy metal/toxin removal measures, targeted supplementation designed to directly support and heal the failing ability of the cardiac mitochondria to produce normal levels of ATP is essential for an optimal cardiac and clinical response.
Even if there is refusal to acknowledge the likely presence of heavy metals in the failing heart muscle, which will continue to be the rule rather than the exception among traditional cardiologists, non-prescription nutrient chelators and ATP production promoters can still be taken as desired, and substantial benefit will result most of the time.
Thomas E Levy MD JD is a former Assistant Professor of Medicine at Tulane Medical School and a past Fellow of the American College of Cardiology. He is also a bar-certified attorney. He can be reached at televymd@yahoo.com. All his articles for the Orthomolecular Medicine News Service can be accessed at https://www.tomlevymd.com/health_ebytes.php.
Note: To access any of the references below, type in the PMID number following the citation in the search box at this link: https://pubmed.ncbi.nlm.nih.gov/.
References
- Brieler J, Breeden M, Tucker J (2017) Cardiomyopathy: an overview. American Family Physician 96:640-646. PMID: https://pubmed.ncbi.nlm.nih.gov/29431384
- Maron B, Towbin J, Thiene G et al. (2006) Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 113:1807-1816. PMID: https://pubmed.ncbi.nlm.nih.gov/16567565
- Elliott P, Andersson B, Arbustini E et al. (2008) Classification of the cardiomyopathies: a position statement from the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. European Heart Journal 29:270-276. PMID: https://pubmed.ncbi.nlm.nih.gov/17916581
- van Deursen V, Damman K, van der Meer P et al. (2014) Co-morbidities in heart failure. Heart Failure Reviews 19:163-172. PMID: https://pubmed.ncbi.nlm.nih.gov/23266884
- Deichl A, Wachter R, Edelmann F (2022) Comorbidities in heart failure with preserved ejection fraction. Herz 47:301-307. PMID: https://pubmed.ncbi.nlm.nih.gov/35674774
- Dorr M, Riemer U, Christ M, et al. (2021) Hospitalizations for heart failure: still major differences between East and West Germany 30 years after reunification. ESC Heart Failure 8:2546-2555. PMID: https://pubmed.ncbi.nlm.nih.gov/33949148
- La Franca E, Manno G, Ajello L et al. (2021) Physiopathology and diagnosis of congestive heart failure: consolidated certainties and new perspectives. Current Problems in Cardiology 46:100691. PMID: https://pubmed.ncbi.nlm.nih.gov/33012532
- Chen J, Aronowitz P (2022) Congestive heart failure. The Medical Clinics of North America 106:447-458. PMID: https://pubmed.ncbi.nlm.nih.gov/35491065
- Borlaug B (2020) Evaluation and management of heart failure with preserved ejection fraction. Nature Reviews: Cardiology 17:559-573. PMID: https://pubmed.ncbi.nlm.nih.gov/32231333
- de Abreu (2022) Heart failure with a preserved ejection fraction and the EMPEROR-Preserved Trial: a review of how we got here. Heart Failure Reviews 27:2077-2082. PMID: https://pubmed.ncbi.nlm.nih.gov/35604573
- Sinatra S (2009) Metabolic cardiology: the missing link in cardiovascular disease. Alternative Therapies in Health and Medicine 15:48-50. PMID: https://pubmed.ncbi.nlm.nih.gov/19284182
- King M, Kingery J, Casey B (2012) Diagnosis and evaluation of heart failure. American Family Physician 85:1161-1168. PMID: https://pubmed.ncbi.nlm.nih.gov/22962896
- Chimenti C, Frustaci A, Pieroni M, Maseri A (1999) Histologically proven myocarditis in patients with biventricular dysfunction and severe asymptomatic coronary artery disease. Cardiologia 44:177-180. PMID: https://pubmed.ncbi.nlm.nih.gov/10208054
- Marin-Garcia J (2016) Cell death in the pathogenesis and progression of heart failure. Heart Failure Reviews 21:117-121. PMID: https://pubmed.ncbi.nlm.nih.gov/26886226
- Tschope C. Ammirati E, Bozkurt B et al. (2021) Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nature Reviews: Cardiology 18:169-193. PMID: https://pubmed.ncbi.nlm.nih.gov/33046850
- Freeman R (1965) Reversible myocarditis due to chronic lead poisoning in childhood. Archives of Disease in Childhood 40:389-393. PMID: https://pubmed.ncbi.nlm.nih.gov/14329255
- Kopp S, Barron J, Tow J (1988) Cardiovascular actions of lead and relationship to hypertension: a review. Environmental Health Perspectives 78:91-99. PMID: https://pubmed.ncbi.nlm.nih.gov/3060356
- Prozialeck W, Edwards J, Nebert D et al. (2008) The vascular system as a target of metal toxicity. Toxicological Sciences 102:207-218. PMID: https://pubmed.ncbi.nlm.nih.gov/17947343
- Read J, Williams J (1952) Lead myocarditis: report of a case. American Heart Journal 44:797-802. PMID: https://pubmed.ncbi.nlm.nih.gov/12985544
- Kline T (1960) Myocardial changes in lead poisoning. A.M.A. Journal of Diseases of Children 99:48-54. PMID: https://pubmed.ncbi.nlm.nih.gov/14409891
- Hegde S, Maysky M, Zaidi A (2020) A rare case of lead-induced cardiomyopathy. JACC: Case Reports 2:1496-1500. PMID: https://pubmed.ncbi.nlm.nih.gov/34317004
- Revis N, Major T, Horton C (1980) The effects of cadmium, magnesium, lead, or cadmium on lipoprotein metabolism and atherosclerosis in the pigeon. Journal of Environmental Pathology and Toxicology 4:293-303. PMID: https://pubmed.ncbi.nlm.nih.gov/7462906
- Webb R, Winquist R, Victery W, Vander A (1981) In vivo and in vitro effects of lead on vascular reactivity in rats. The American Journal of Physiology 241:H211-H216. PMID: https://pubmed.ncbi.nlm.nih.gov/7270708
- Revis N, Zinsmeister A, Bull R (1981) Atherosclerosis and hypertension induction by lead and cadmium ions: an effect prevented by calcium ion. Proceedings of the National Academy of Sciences of the United States of America 78:6494-6498. PMID: https://pubmed.ncbi.nlm.nih.gov/6947240
- Levy T (2023) https://www.tomlevymd.com/articles/omns20230731/The-Toxic-Nutrient-Triad
- Shokrzadeh M, Ghaemian A, Salehifar E et al. (2009) Serum zinc and copper levels in ischemic cardiomyopathy. Biological Trace Element Research 127:116-123. PMID: https://pubmed.ncbi.nlm.nih.gov/18953508
- Cheung C, Soon C, Chuang C et al. (2015) Low-dose copper infusion into the coronary circulation induces acute heart failure in diabetic hearts: new mechanism of heart disease. Biochemical Pharmacology 97:62-76. PMID: https://pubmed.ncbi.nlm.nih.gov/26208785
- Reid A, Miller C, Farrant J et al. (2022) Copper chelation in patients with hypertrophic cardiomyopathy. Open Heart 9:e001803. PMID: https://pubmed.ncbi.nlm.nih.gov/35169044
- Cooper G, Young A, Gamble G et al. (2009) A copper(II)-selective chelator ameliorates left-ventricular hypertrophy in type 2 diabetes patients: a randomized placebo-controlled study. Diabetologia 52:715-722. PMID: https://pubmed.ncbi.nlm.nih.gov/19172243
- Cooper G, Phillips A, Choong et al. (2004) Regeneration of the heart in diabetes by selective copper chelation. Diabetes 53:2501-2508. PMID: https://pubmed.ncbi.nlm.nih.gov/15331567
- Lu J, Pontre B, Pickup S et al. (2013) Treatment with a copper-selective chelator causes substantive improvement in cardiac function of diabetic rats with left-ventricular impairment. Cardiovascular Diabetology 12:28. PMID: https://pubmed.ncbi.nlm.nih.gov/23368770
- Baynes J, Murray D (2009) The metal chelators, trientine and citrate, inhibit the development of cardiac pathology in the Zucker diabetic rat. Experimental Diabetes Research 2009:696376. PMID: https://pubmed.ncbi.nlm.nih.gov/19390595
- Muers M, Stokes W (1976) Treatment of scleroderma heart by D-penicillamine. British Heart Journal 38:864-867. PMID: https://pubmed.ncbi.nlm.nih.gov/135572
- Zheng Y, Li X, Wang Y, Cai L (2008) The role of zinc, copper and iron in the pathogenesis of diabetes and diabetic complications: therapeutic effects by chelators. Hemoglobin 32:135-145. PMID: https://pubmed.ncbi.nlm.nih.gov/18274991
- Cooper G (2011) Therapeutic potential of copper chelation with triethylenetetramine in managing diabetes mellitus and Alzheimer's disease. Drugs 71:1281-1320. PMID: https://pubmed.ncbi.nlm.nih.gov/21770477
- Yin J, Sun L, Zheng J et al. (2016) Copper chelation by trientine dihydrochloride inhibits liver RFA-induced inflammatory responses in vivo. Inflammation Research 65:1009-1020. PMID: https://pubmed.ncbi.nlm.nih.gov/27613237
- Rahko P, Salemi R, Uretsky B (1986) Successful reversal of chelation therapy of congestive cardiomyopathy due to iron overload. Journal of the American College of Cardiology 8:436-440. PMID: https://pubmed.ncbi.nlm.nih.gov/3734266
- Mancuso L, Iacona M, Marchi S et al. (1985) [Severe cardiomyopathy in a woman with intermediate beta-thalassemia. Regression of cardiac failure with desferrioxamine.] Article in Italian. Giornale Italiano di Cardiologia 15:916-920. PMID: https://pubmed.ncbi.nlm.nih.gov/4085735
- Gulati V, Harikrishnan P, Palaniswamy C et al. (2014) Cardiac involvement in hemochromatosis. Cardiology in Review 22:56-68. PMID: https://pubmed.ncbi.nlm.nih.gov/24503941
- Kumfu S, Chattipakorn S, Fucharoen S, Chattipakorn N (2012) Mitochondrial calcium uniporter blocker prevents cardiac mitochondrial dysfunction induced by iron overload in thalassemic mice. Biometals 25:1167-1175. PMID: https://pubmed.ncbi.nlm.nih.gov/22910858
- Ju H, Liu T, Yang M et al. (2023) Iron and atrial fibrillation: a review. Pacing and Clinical Electrophysiology 46:312-318. PMID: https://pubmed.ncbi.nlm.nih.gov/36799332
- Khamseekaew J, Kumfu S, Wongjaikam S et al. (2017) Effects of iron overload, an iron chelator and a T-type calcium channel blocker on cardiac mitochondrial biogenesis and mitochondrial dynamics in thalassemic mice. European Journal of Pharmacology 799:118-127. PMID: https://pubmed.ncbi.nlm.nih.gov/28192097
- Kumfu S, Chattipakorn S, Chattipakorn N (2022) Iron overload cardiomyopathy: using the latest evidence to inform future applications. Experimental Biology and Medicine 247:574-583. PMID: https://pubmed.ncbi.nlm.nih.gov/35130741
- Das S, Wang W, Zhabyeyev P et al. (2015) Iron-overload injury and cardiomyopathy in acquired and genetic models is attenuated by resveratrol therapy. Scientific Reports 5:18132. PMID: https://pubmed.ncbi.nlm.nih.gov/26638758
- Das S, DesAulniers J, Dyck J et al. (2016) Resveratrol mediates therapeutic hepatic effects in acquired and genetic models of iron-overload. Liver International 36:246-257. PMID: https://pubmed.ncbi.nlm.nih.gov/26077449
- Das S, Zhabyeyev P, Basu R et al. (2018) Advanced iron-overload cardiomyopathy in a genetic murine model is rescued by resveratrol therapy. Bioscience Reports 38:BSR20171302. PMID: https://pubmed.ncbi.nlm.nih.gov/29208771
- Sumneang N, Kumfu S, Khamseekaew J et al. (2019) Combined iron chelator with N-acetylcysteine exerts the greatest effect on improving cardiac calcium homeostasis in iron-overloaded thalassemic mice. Toxicology 427:152289. PMID: https://pubmed.ncbi.nlm.nih.gov/31542421
- Frustaci A, Magnavita N, Chimenti C et al. (1999) Marked elevation of myocardial trace elements in idiopathic dilated cardiomyopathy compared with secondary cardiac dysfunction. Journal of the American College of Cardiology 33:1578-1583. PMID: https://pubmed.ncbi.nlm.nih.gov/10334427
- Baldwin D, Marshsall W (1999) Heavy metal poisoning and its laboratory investigation. Annals of Clinical Biochemistry 36(Pt 3):267-300. PMID: https://pubmed.ncbi.nlm.nih.gov/10376071
- Cirovic Ana, Dordevic A, Cirovic A et al. (2023) Trace element concentrations in autopsied heart tissues from patients with secondary cardiomyopathy. Biological Trace Element Research Sep 25. Online ahead of print. PMID: https://pubmed.ncbi.nlm.nih.gov/37747654
- Cooper L, Rader V, Ralston N (2007) The roles of selenium and mercury in the pathogenesis of viral cardiomyopathy. Congestive Heart Failure 13:193-199. PMID: https://pubmed.ncbi.nlm.nih.gov/17673870
- Caforio A, Mahon N, Tona F, McKenna W (2002) Circulating cardiac autoantibodies in dilated cardiomyopathy and myocarditis: pathogenetic and clinical significance. European Journal of Heart Failure 4:411-417. PMID: https://pubmed.ncbi.nlm.nih.gov/12167378
- Ilback N, Lindh U, Fohlman J, Friman G (1995) New aspects of murine coxsackie B3 myocarditis-focus on heavy metals. European Heart Journal 16 Suppl O:20-24. PMID: https://pubmed.ncbi.nlm.nih.gov/8682094
- Reeves W, Marcuard S, Willis S, Movahed A (1989) Reversible cardiomyopathy due to selenium deficiency. JPEN: Journal of Parenteral and Enteral Nutrition 13:663-665. PMID: https://pubmed.ncbi.nlm.nih.gov/2614867
- Yusuf S. Rehman Q, Casscells W (2002) Cardiomyopathy in association with selenium deficiency: a case report. JPEN: Journal of Parenteral and Enteral Nutrition 26:63-66. PMID: https://pubmed.ncbi.nlm.nih.gov/11833754
- Munguti C, Rifai M, Shaheen W (2017) A rare cause of cardiomyopathy: a case of selenium deficiency causing severe cardiomyopathy that improved on supplementation. Cureus 9:e1627. PMID: https://pubmed.ncbi.nlm.nih.gov/29098137
- Spiller H (2018) Rethinking mercury: the role of selenium in the pathophysiology of mercury toxicity. Clinical Toxicity 56:313-326. PMID: https://pubmed.ncbi.nlm.nih.gov/29124976
- Petrovic M, Otero D, Leigh A, Singh V (2021) Acute heart failure due to aluminum phosphide poisoning. Methodist DeBakey Cardiovascular Journal 17:6-12. PMID: https://pubmed.ncbi.nlm.nih.gov/34824673
- Akkaoui M, Achour S, Abidi K et al. (2007) Reversible myocardial injury associated with aluminum phosphide poisoning. Clinical Toxicology 45:728-731. PMID: https://pubmed.ncbi.nlm.nih.gov/17849252
- Elabbassi W, Chowdhury M, Fachtartz A (2014) Severe reversible myocardial injury associated with aluminum phosphide toxicity: a case report and review of literature. Journal of the Saudi Heart Association 26:216-221. PMID: https://pubmed.ncbi.nlm.nih.gov/25278724
- Roth A, Nogues C, Galle P, Drueke T (1984) Multiorgan aluminum deposits in chronic haemodialysis patient. Electron microscope and microprobe studies. Virchows Archiv. A, Pathological Anatomy and Histopathology 405:131-140. PMID: https://pubmed.ncbi.nlm.nih.gov/6438896
- Galal S, Hasan H, Abdel-Rafei M, Kiki S (2019) Synergistic effect of cranberry extract and losartan against aluminum chloride-induced hepatorenal damage associated cardiomyopathy in rats. Archives of Physiology and Biochemistry 125:357-366. PMID: https://pubmed.ncbi.nlm.nih.gov/29685075
- Domingo J (1989) The use of chelating agents in the treatment of aluminum overload. Journal of Toxicology: Clinical Toxicology 27:355-367. PMID: https://pubmed.ncbi.nlm.nih.gov/2697761
- Giacon G, Boon K (2021) Cobalt toxicity: a preventable and treatable cause for possibly life threatening cardiomyopathy. The New Zealand Medical Journal 134:103-108. PMID: https://pubmed.ncbi.nlm.nih.gov/33582712
- Umar M, Jahangir N, Khan M et al. (2020) Cobalt-related cardiomyopathy: a real concern! A review of published evidence. Journal of Orthopaedic Surgery 28:2309499020905993. PMID: https://pubmed.ncbi.nlm.nih.gov/32410523
- Fung E. Monnot A, Kovochich M et al. (2018) Characteristics of cobalt-related cardiomyopathy in metal hip implant patients: an evaluation of 15 published reports. Cardiovascular Toxicology 18:206-220. PMID: https://pubmed.ncbi.nlm.nih.gov/29188590
- Bradberry S, Wilkinson J, Ferner R (2014) Systemic toxicity related to metal hip prostheses. Clinical Toxicology 52:837-847. PMID: https://pubmed.ncbi.nlm.nih.gov/25132471
- Jenkinson M, Meek R, Tate R et al. (2021) Cobalt-induced cardiomyopathy-do circulating cobalt levels matter? Bone & Joint Research 10:340-347. PMID: https://pubmed.ncbi.nlm.nih.gov/34053230
- Rona G (1971) Experimental aspects of cobalt cardiomyopathy. British Heart Journal 33(Suppl):171-174. PMID: https://pubmed.ncbi.nlm.nih.gov/5572639
- Giampreti A, Lonati D, Ragghianti B et al. (2016) N-acetyl-cysteine as effective and safe chelating agent in metal-on-metal hip-implanted patients: two cases. Case Reports in Orthopedics 2016:8682737. PMID: https://pubmed.ncbi.nlm.nih.gov/27148463
- Webb M (1962) The biological action of cobalt and other metals. III. Chelation of cations by dihydrolipoic acid. Biochimica et Biophysica Acta 65:47-65. PMID: https://pubmed.ncbi.nlm.nih.gov/13999338
- Smetana R, Glogar D, Gemeiner M (1985) [Heavy metal and trace element concentrations in patients with idiopathic dilated cardiomyopathy.] Article in German. Weiner Klinische Wochenschrift 97:697-701. PMID: https://pubmed.ncbi.nlm.nih.gov/4060731
- Archer S (2008) Dilated cardiomyopathy and left bundle branch block associated with ingestion of colloidal gold and silver is reversed by British antiLewisite and vitamin E: the potential toxicity of metals used as health supplements. The Canadian Journal of Cardiology 24:397-399. PMID: https://pubmed.ncbi.nlm.nih.gov/18464946
- Bloom M, Harno C, Cardinale D et al. (2016) Cancer therapy-related cardiac dysfunction and heart failure: Part 1: definitions, pathophysiology, risk factors, and imaging. Circulation: Heart Failure 9:e002661. PMID: https://pubmed.ncbi.nlm.nih.gov/26747861
- Hamo C, Bloom M, Cardinale D et al. (2016) Cancer therapy-related cardiac dysfunction and heart failure: Part 2: prevention, treatment, guidelines, and future directions. Circulation: Heart Failure 9:e002843. PMID: https://pubmed.ncbi.nlm.nih.gov/26839395
- Keefe D (2001) Anthracycline-induced cardiomyopathy. Seminars in Oncology 28:2-7. PMID: https://pubmed.ncbi.nlm.nih.gov/11552224
- Sauer H (1997) [The prevention of anthracycline-induced cardiomyopathy with a chelating agent (dexrazoxane = ICRF-187).] Article in German. Strahlentherapie und Oncologie 173:51-51. PMID: https://pubmed.ncbi.nlm.nih.gov/9082586
- Higgins A, O'Halloran T, Chang J (2015) Chemotherapy-induced cardiomyopathy. Heart Failure Reviews 20:721-730. PMID: https://pubmed.ncbi.nlm.nih.gov/26338137
- Hellmann K (1996) Cardioprotection by dexrazoxane (Cardioxane; ICRF 187): progress in supportive care. Supportive Care in Cancer 4:305-307. PMID: https://pubmed.ncbi.nlm.nih.gov/8829310
- Levy T (2023) https://www.tomlevymd.com/articles/omns20230310/Resolving-Persistent-Spike-Protein-Syndrome
- Levy T (2023) https://www.tomlevymd.com/articles/omns20230927/Persistent-Spike-Protein-Syndrome:-Rapid-Resolution-with-Ultraviolet-Blood-Irradiation
- Levy T (2021) https://www.tomlevymd.com/articles/omns20211018/Canceling-the-Spike-Protein:-Striking-Visual-Evidence
- Levy T (2023) https://www.tomlevymd.com/articles/omns20230105/Myocarditis:-Once-Rare-Now-Common
- Parry P, Lefringhausen A, Turni C et al. (2023) "Spikeopathy": COVID-19 spike protein is pathogenic, from both virus and vaccine mRNA. Biomedicines 11:2287. PMID: https://pubmed.ncbi.nlm.nih.gov/37626783
- Ondruschka B, Heinrich F, Lindenmeyer M et al. (2021) Multiorgan tropism of SARS-CoV-2 lineage B.1.1.7. International Journal of Legal Medicine 135:2347-2349. PMID: https://pubmed.ncbi.nlm.nih.gov/34486072
- Ping H, Zhang K, Wang Y et al. (2021) Cell death and pathological findings of the spleen in COVID-19 patients. Pathology, Research, and Practice 227:153610. PMID: https://pubmed.ncbi.nlm.nih.gov/34601398
- Morz M (2022) A case report: multifocal necrotizing encephalitis and myocarditis after BNT162b2 mRNA vaccination against COVID-19. Vaccines 10:1651. PMID: https://pubmed.ncbi.nlm.nih.gov/36298516
- Macedo S, Pestana A, Santos L et al. (2022) Detection of SARS-CoV-2 infection in thyroid follicular cells from a COVID-19 autopsy series. European Thyroid Journal 11:e220074. PMID: https://pubmed.ncbi.nlm.nih.gov/35900859
- Shang J, Wan Y, Luo C et al. (2020) Cell entry mechanisms of SARS-CoV-2. Proceedings of the National Academy of Sciences of the United States of America 117:11727-11734. PMID: https://pubmed.ncbi.nlm.nih.gov/32376634
- Pillay T (2020) Gene of the month: the 2019-nCoV/SARS-CoV-2 novel coronavirus spike protein. Journal of Clinical Pathology 73:366-369. PMID: https://pubmed.ncbi.nlm.nih.gov/32376714
- Belouzard S, Millet J, Licitra B, Whittaker G (2012) Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses 4:1011-1033. PMID: https://pubmed.ncbi.nlm.nih.gov/22816037
- Uversky V, Redwan E, Makis W, Rubio-Casillas A (2023) IgG4 antibodies induced by repeated vaccination may generate immune tolerance to the SARS-CoV-2 spike protein. Vaccines 11:991. PMID: https://pubmed.ncbi.nlm.nih.gov/37243095
- Gusev E, Sarapultsev A, Solomatina L, Chereshnev V (2022) SARS-CoV-2-specific immune response and the pathogenesis of COVID-19. International Journal of Molecular Sciences 23:1716. PMID: https://pubmed.ncbi.nlm.nih.gov/35163638
- Theoharides T (2022) Could SARS-CoV-2 spike protein be responsible for long-COVID syndrome? Molecular Neurobiology 59:1850-1861. PMID: https://pubmed.ncbi.nlm.nih.gov/35028901
- Biswas S, Thakur V, Kaur P et al. (2021) Blood clots in COVID-19 patients: simplifying the curious mystery. Medical Hypotheses 146:110371. PMID: https://pubmed.ncbi.nlm.nih.gov/33223324
- Zhang S, Liu Y, Wang K et al. (2020) SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. Journal of Hematology & Oncology 13:120. PMID: https://pubmed.ncbi.nlm.nih.gov/32887634
- Cao S, Song Z, Rong J et al. (2023) Spike protein fragments promote Alzheimer's amyloidogenesis. ACS Applied Materials & Interfaces 15:40317-40329. PMID: https://pubmed.ncbi.nlm.nih.gov/37585091
- Seneff S, Kyriakopoulos A, Nigh G, McCullough P (2023) A potential role of the spike protein in neurodegenerative diseases: a narrative review. Cureus 15:e34872. PMID: https://pubmed.ncbi.nlm.nih.gov/36788995
- Fernandes B, Feitosa N, Barbosa A et al. (2022) Toxicity of spike fragments SARS-CoV-2 S protein for zebrafish: a tool to study its hazardous for human health? The Science of the Total Environment 813:152345. PMID: https://pubmed.ncbi.nlm.nih.gov/34942250
- Alden M, Falla F, Yang D et al. (2022) Intracellular reverse transcription of Pfizer BioNTech COVID-19 mRNA vaccine BNT162b2 in vitro in human lever cell line. Current Issues in Molecular Biology 44:1115-1126. PMID: https://pubmed.ncbi.nlm.nih.gov/35723296
- Haslbauer J, Tzankov A, Mertz K et al. (2021) Characterisation of cardiac pathology in 23 autopsies of lethal COVID-19. The Journal of Pathology: Clinical Research 7:326-337. PMID: https://pubmed.ncbi.nlm.nih.gov/33837673
- Lindner D, Fitzek A, Brauninger H et al. (2020) Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiology 5:1281-1285. PMID: https://pubmed.ncbi.nlm.nih.gov/32730555
- Bielecka-Dabrowa A, Cichocka-Radwan A, Lewek J et al. (2021) Cardiac manifestations of COVID-19. Reviews in Cardiovascular Medicine 22:365-371. PMID: https://pubmed.ncbi.nlm.nih.gov/34258904
- Jakovac H, Ferencic A, Stemberger C et al. (2022) Detection of SARS-CoV-2 antigens in the AV-node of a cardiac conduction system-a case report. Tropical Medicine and Infectious Diseases 7:43. PMID: https://pubmed.ncbi.nlm.nih.gov/35324590
- Choi S, Lee S, Seo J et al. (2021) Myocarditis-induced sudden death after BNT162b2 mRNA COVID-19 vaccination in Korea: case report focusing on histopathological findings. Journal of Korean Medical Science 36:e286. PMID: https://pubmed.ncbi.nlm.nih.gov/34664804
- Fox S, Akmatbekov A, Harbert J et al. (2020) Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. The Lancet: Respiratory Medicine 8:681-686. PMID: https://pubmed.ncbi.nlm.nih.gov/32473124
- Jum'ah H, Loeffler A, Tomasshefski Jr J (2021) Histopathological findings in the hearts of COVID-19 autopsies: a letter to Cardiovascular Pathology journal editor in response to Halushka et al. 2020. Cardiovascular Pathology 52:107333. PMID: https://pubmed.ncbi.nlm.nih.gov/33741530
- Nedeljkovic I, Giga V, Ostojic M et al. (2021) Focal myocarditis after mild COVID-19 infection in athletes. Diagnostics 11:1519. PMID: https://pubmed.ncbi.nlm.nih.gov/34441453
- Hantson P (2019) Mechanisms of toxic cardiomyopathy. Clinical Toxicology 57:1-9. PMID: https://pubmed.ncbi.nlm.nih.gov/30260248
- Levy T (2019) Magnesium, Reversing Disease, Henderson, NV: MedFox Publishing [Free eBook download available at https://mag.medfoxpub.com/]
- Levy T (2013) Death by Calcium: Proof of the toxic effects of dairy and calcium supplements, Henderson, NV: MedFox Publishing [Free eBook download available at https://dbc2.medfoxpub.com/]
- Sabbah H (2020) Targeting the mitochondria in heart failure: a translational perspective. JACC: Basic to Translational Science 5:88-106. PMID: https://pubmed.ncbi.nlm.nih.gov/32043022
- Ventura-Clapier R, Garnier A, Veksler V, Joubert F (2011) Bioenergetics of the failing heart. Biochimica et Biophysica Acta 1813:1360-1372. PMID: https://pubmed.ncbi.nlm.nih.gov/20869993
- Peoples J, Saraf A, Ghazal N et al. (2019) Mitochondrial dysfunction and oxidative stress in heart disease. Experimental & Molecular Medicine 51:1-13. PMID: https://pubmed.ncbi.nlm.nih.gov/31857574
- Sinatra S (2009) Metabolic cardiology: an integrative strategy in the treatment of congestive heart failure. Alternative Therapies in Health and Medicine 15:44-52. PMID: https://pubmed.ncbi.nlm.nih.gov/19472864
- Danieli M, Antonelli E, Piga M et al. (2023) Oxidative stress, mitochondrial dysfunction, and respiratory chain enzyme defects in inflammatory myopathies. Autoimmunity Reviews 22:103308. PMID: https://pubmed.ncbi.nlm.nih.gov/36822387
- El-Hattab A, Scaglia F (2016) Mitochondrial cardiomyopathies. Frontiers in Cardiovascular Medicine 3:25. PMID: https://pubmed.ncbi.nlm.nih.gov/27504452
- Nolfi-Donegan D, Braganza A, Shiva S (2020) Mitochondrial electron transport chain: oxidative phosphorylation, oxidant production, and methods of measurement. Redox Biology 37:101674. PMID: https://pubmed.ncbi.nlm.nih.gov/32811789
- Lesnefsky E, Chen Q, Hoppel C (2016) Mitochondrial metabolism in aging heart. Circulation Research 118:1593-1611. PMID: https://pubmed.ncbi.nlm.nih.gov/27174952
- Berthiaume J, Kurdys J, Muntean D, Rosca M (2019) Mitochondrial NAD+/NADH redox state and diabetic cardiomyopathy. Antioxidants & Redox Signaling 30:375-398. PMID: https://pubmed.ncbi.nlm.nih.gov/29073779
- Chen Z, Jin Z, Cai J et al. (2022) Energy substrate metabolism and oxidative stress in metabolic cardiomyopathy. Journal of Molecular Medicine 100:1721-1739. PMID: https://pubmed.ncbi.nlm.nih.gov/36396746
- Alehagen U, Aaseth J, Alexander J, Johansson P (2018) Still reduced cardiovascular mortality 12 years after supplementation with selenium and coenzyme Q10 for four years: a validation of previous 10-year follow-up results of a prospective randomized double-blind placebo-controlled trial in elderly. PLoS One 13:e0193120. PMID: https://pubmed.ncbi.nlm.nih.gov/29641571
- Casademont J, Miro O (2002) Electron transport chain defects in heart failure. Heart Failure Reviews 7:131-139. PMID: https://pubmed.ncbi.nlm.nih.gov/11988637
- Brown D, Perry J, Allen M et al. (2017) Expert consensus document: mitochondrial function as a therapeutic target in heart failure. Nature Reviews: Cardiology 14:238-250. PMID: https://pubmed.ncbi.nlm.nih.gov/28004807
- Meyers D, Basha H, Koenig M (2013) Mitochondrial cardiomyopathy: pathophysiology, diagnosis, and management. Texas Heart Institute Journal 40:385-394. PMID: https://pubmed.ncbi.nlm.nih.gov/24082366
- Ernster L, Daliner G (1995) Biochemical, physiological and medical aspects of ubiquinone function. Biochimica et Biophysica Acta 1271:195-204. PMID: https://pubmed.ncbi.nlm.nih.gov/7599208
- Mortensen S, Rosenfeldt F, Kumar A et al. (2014) The effect of coenzyme Q10 on morbidity and mortality in chronic heart failure: results from Q-SYMBIO: a randomized double-blind trial. JACC: Heart Failure 2:641-649. PMID: https://pubmed.ncbi.nlm.nih.gov/25282031
- Alehagen U, Johansson P, Bjornstedt M et al. (2013) Cardiovascular mortality and N-terminal-proBNP reduced after combined selenium and coenzyme Q10 supplementation: a 5-year prospective randomized double-blind placebo-controlled trial among elderly Swedish citizens. International Journal of Cardiology 167:1860-1866. PMID: https://pubmed.ncbi.nlm.nih.gov/22626835
- Sacher H, Sacher M, Landau S et al. (1997) The clinical and hemodynamic effects of coenzyme Q10 in congestive cardiomyopathy. American Journal of Therapeutics 4:66-72. PMID: https://pubmed.ncbi.nlm.nih.gov/10423594
- Fotino A, Thompson-Paul A, Bazzano L (2013) Effect of Coenzyme Q10 supplementation on heart failure: a meta-analysis. The American Journal of Clinical Nutrition 97:268-275. PMID: https://pubmed.ncbi.nlm.nih.gov/23221577
- Langsjoen P, Folkers K, Lyson K et al. (1990) Pronounced increase in survival of patients with cardiomyopathy when treated with coenzyme Q10 and conventional therapy. International Journal of Tissue Reactions 12:163-168. PMID: https://pubmed.ncbi.nlm.nih.gov/2276894
- Langsjoen P, Langsjoen A, Folkers K (1990) A six-year clinical study of therapy of cardiomyopathy with coenzyme Q10. International Journal of Tissue Reactions 12:169-171. PMID: https://pubmed.ncbi.nlm.nih.gov/2276895
- Langsjoen P, Langsjoen A (2008) Supplemental ubiquinol in patients with advanced congestive heart failure. Biofactors 32:119-128. PMID: https://pubmed.ncbi.nlm.nih.gov/19096107
- Sharma A, Fonarow G, Butler J et al. (2016) Coenzyme Q10 and heart failure: a state-of-the-art review. Circulation: Heart Failure 9:e002639. PMID: https://pubmed.ncbi.nlm.nih.gov/27012265
- Sobirin M, Herry Y, Sofia S et al. (2019) Effects of coenzyme Q10 supplementation on diastolic function in patients with heart failure with preserved ejection fraction. Drug Discoveries & Therapeutics 13:38-46. PMID: https://pubmed.ncbi.nlm.nih.gov/30880321
- Langsjoen P, Langsjoen A, Willis R, Folkers K (1997) Treatment of hypertrophic cardiomyopathy with coenzyme Q10. Molecular Aspects of Medicine 18 Suppl:S145-S151. PMID: https://pubmed.ncbi.nlm.nih.gov/9266516
- Senes M, Erbay A, Yilmaz F et al. (2008) Coenzyme Q10 and high-sensitivity C-reactive protein in ischemic and idiopathic dilated cardiomyopathy. Clinical Chemistry and Laboratory Medicine 46:382-386. PMID: https://pubmed.ncbi.nlm.nih.gov/18254715
- Molyneux S, Florkowski C, George P et al. (2008) Coenzyme Q10: an independent predictor of mortality in chronic heart failure. Journal of the American College of Cardiology 52:1435-1441. PMID: https://pubmed.ncbi.nlm.nih.gov/19017509
- Shimizu M, Miyazaki T, Takagi A et al. (2021) Low coenzyme Q10 levels in patients with acute cardiovascular disease are associated with long-term mortality. Heart Vessels 36:401-407. PMID: https://pubmed.ncbi.nlm.nih.gov/32939561
- Oleck S, Ventura H (2016) Coenzyme Q10 and utility in heart failure: just another supplement? Current Heart Failure Reports 13:190-195. PMID: https://pubmed.ncbi.nlm.nih.gov/27333901
- An P, Wan S, Luo Y et al. (2022) Micronutrient supplementation to reduce cardiovascular risk. Journal of the American College of Cardiology 80:2269-2285. PMID: https://pubmed.ncbi.nlm.nih.gov/36480969
- Lei L, Liu Y (2017) Efficacy of coenzyme Q10 in patients with cardiac failure: a meta-analysis of clinical trials. BMC Cardiovascular Disorders 17:196. PMID: https://pubmed.ncbi.nlm.nih.gov/28738783
- Di Lorenzo A, Iannuzzo G, Parlato A et al. (2020) Clinical evidence for Q10 coenzyme supplementation in heart failure: from energetics to functional improvement. Journal of Clinical Medicine 9:1266. PMID: https://pubmed.ncbi.nlm.nih.gov/32349341
- Ayer A, Macdonald P, Stocker R (2015) CoQ10 function and role in heart failure and ischemic heart disease. Annual Review of Nutrition 35:175-213. PMID: https://pubmed.ncbi.nlm.nih.gov/25974695
- Goldman L, Schafer A (2019) Goldman-Cecil Medicine, 26th edition, Elsevier Publishing
- Ancha S, Auberle C, Cash D et al. (2022) The Washington Manual of Medical Therapeutics, 37th edition, Lippincott Williams & Wilkins Publisher
- Festenstein G, Heaton F, Lowe J, Morton R (1955) A constituent of the unsaponifiable portion of animal tissue lipids (lambdamax. 272 mµ). The Biochemical Journal 59:558-566. PMID: https://pubmed.ncbi.nlm.nih.gov/14363147
- Crane F, Hatefi Y, Lester R, Widmer C (1957) Isolation of a quinone from beef heart mitochondria. Biochimica et Biophysica Acta 25:220-221. PMID: https://pubmed.ncbi.nlm.nih.gov/13445756
- Maes M, Mihaylova I, Kubera M et al. (2009) Lower plasma coenzyme Q10 in depression: a marker for treatment resistance and chronic fatigue in depression and a risk factor to cardiovascular disorder in that illness. Neuro Endocrinology Letters 30:462-469. PMID: https://pubmed.ncbi.nlm.nih.gov/20010493
- Nikolaevna O, Aronovna G, Igorevna K et al. (2020) Intravenous administration of coenzyme Q10 in acute period of cerebral ischemia decreases mortality by reducing brain necrosis and limiting its increase within 4 days in rat stroke model. Antioxidants 9:1240. PMID: https://pubmed.ncbi.nlm.nih.gov/33297323
- Manzar H, Abdulhussein D, Yap T, Cordeiro M (2020) Cellular consequences of coenzyme Q10 deficiency in neurodegeneration of the retina and brain. International Journal of Molecular Sciences 21:9299. PMID: https://pubmed.ncbi.nlm.nih.gov/33291255
- Rauchova H (2021) Coenzyme Q10 effects in neurological diseases. Physiological Research 70:S683-S714. PMID: https://pubmed.ncbi.nlm.nih.gov/35199552
- Gvozdjakova A, Kucharska J, Ostatnikova D et al. (2014) Ubiquinol improves symptoms in children with autism. Oxidative Medicine and Cellular Longevity 2014:798957. PMID: https://pubmed.ncbi.nlm.nih.gov/24707344
- Gamal F, Agami O, Salamah A (2022) Coenzyme Q10 in the treatment of attention deficit hyperactivity disorder in children: a randomized controlled trial. CNS & Neurological Disorders-Drug Targets 21:717-723. PMID: https://pubmed.ncbi.nlm.nih.gov/34819012
- Burke B, Neuenschwander R, Olson R (2001) Randomized, double-blind, placebo-controlled trial of coenzyme Q10 in isolated systolic hypertension. Southern Medical Journal 94:1112-1117. PMID: https://pubmed.ncbi.nlm.nih.gov/11780680
- Rosenfeldt F, Hilton D, Pepe S, Krum H (2003) Systematic review of effect of coenzyme Q10 in physical exercise, hypertension and heart failure. Biofactors 18:91-100. PMID: https://pubmed.ncbi.nlm.nih.gov/14695924
- Rosenfeldt F, Haas S, Krum H et al. (2007) Coenzyme Q10 in the treatment of hypertension: a meta-analysis of the clinical trials. Journal of Human Hypertension 21:297-306. PMID: https://pubmed.ncbi.nlm.nih.gov/17287847
- Yang Y, Wang L, Chen L et al. (2015) Coenzyme Q10 treatment of cardiovascular disorders of ageing including heart failure, hypertension and endothelial dysfunction. Clinica Chimica Acta 450:83-89. PMID: https://pubmed.ncbi.nlm.nih.gov/26254995
- Singh R, Wander G, Rastogi A et al. (1998) Randomized, double-blind placebo-controlled trial of coenzyme Q10 in patients with acute myocardial infarction. Cardiovascular Drugs and Therapy 12:347-353. PMID: https://pubmed.ncbi.nlm.nih.gov/9825179
- Yalcin A, Kilinc E, Sagcan A, Kultursay H (2004) Coenzyme Q10 concentrations in coronary artery disease. Clinical Biochemistry 37:706-709. PMID: https://pubmed.ncbi.nlm.nih.gov/15302616
- Rabanal-Ruiz Y, Llanos-Gonzalez E, Alcain F (2021) The use of coenzyme Q10 in cardiovascular diseases. Antioxidants 10:755. PMID: https://pubmed.ncbi.nlm.nih.gov/34068578
- Shah I, Memon M, Ansari S et al. (2021) Role of coenzyme Q10 in prophylaxis of myocardial infarction. Cureus 13:e13137. PMID: https://pubmed.ncbi.nlm.nih.gov/33728151
- Huang C, Kuo C, Huang C et al. (2016) High plasma coenzyme Q10 concentration is correlated with good left ventricular performance after primary angioplasty in patients with acute myocardial infarction. Medicine 95:e4501. PMID: https://pubmed.ncbi.nlm.nih.gov/27495100
- Makhija N, Sendasgupta C, Kiran U et al. (2008) The role of oral coenzyme Q10 in patients undergoing coronary artery bypass graft surgery. Journal of Cardiothoracic and Vascular Anesthesia 22:832-839. PMID: https://pubmed.ncbi.nlm.nih.gov/18834786
- Zhao Q, Kebbati A, Zhang Y et al. (2015) Effect of coenzyme Q10 on the incidence of atrial fibrillation in patients with heart failure. Journal of Investigative Medicine 63:735-739. PMID: https://pubmed.ncbi.nlm.nih.gov/25919281
- Comhair S, Grandon D, Khan A et al. (2015) Coenzyme Q in asthma. American Journal of Respiratory and Critical Care Medicine 191:1336-1338. PMID: https://pubmed.ncbi.nlm.nih.gov/26029840
- Gazdik F, Gvozdjakova A, Nadvornikova R et al. (2002) Decreased levels of coenzyme Q(10) in patients with bronchial asthma. Allergy 57:811-814. PMID: https://pubmed.ncbi.nlm.nih.gov/12169177
- Bour S, Carmona M, Galinier A et al. (2011) Coenzyme Q as an antiadipogenic factor. Antioxidants & Redox Signaling 14:403-413. PMID: https://pubmed.ncbi.nlm.nih.gov/21091355
- Sawaddiruk P, Apaijai N, Paiboonworachat S et al. (2019) Coenzyme Q10 supplementation alleviates pain in pregabalin-treated fibromyalgia patients via reducing brain activity and mitochondrial dysfunction. Free Radical Research 53:901-909. PMID: https://pubmed.ncbi.nlm.nih.gov/31387429
- Ahmadvand H, Ghasemi-Dehnoo M (2014) Antiatherogenic, hepatoprotective, and hypolipidemic effects of coenzyme Q10 in alloxan-induced type 1 diabetic rats. ARYA Atherosclerosis 10:192-198. PMID: https://pubmed.ncbi.nlm.nih.gov/25258634
- Desbats M, Vetro A, Limongelli I et al. (2015) Primary coenzyme Q10 deficiency presenting as fatal neonatal multiorgan failure. European Journal of Human Genetics 23:1254-1258. PMID: https://pubmed.ncbi.nlm.nih.gov/25564041
- Yeung C, Billings 4th F, Claessens A et al. (2015) Coenzyme Q10 dose-escalation study in hemodialysis patients: safety, tolerability, and effect of oxidative stress. BMC Nephrology 16:183. PMID: https://pubmed.ncbi.nlm.nih.gov/26531095
- De Benedetto F, Pastorelli R, Ferrario M et al. (2018) Supplementation with Qter(r) and creatine improves functional performance in COPD patients on long term oxygen therapy. Respiratory Medicine 142:86-93. PMID: https://pubmed.ncbi.nlm.nih.gov/30170808
- Farhangi M, Alipour B, Jafarvand E, Khoshbaten M (2014) Oral coenzyme Q10 supplementation in patients with nonalcoholic fatty liver disease: effects on serum vaspin, chemerin, pentraxin 3, insulin resistance and oxidative stress. Archives of Medical Research 45:589-595. PMID: https://pubmed.ncbi.nlm.nih.gov/25450583
- Gutierrez-Mariscal F, Arenas-de Larriva A, Limia-Perez L et al. (2020) Coenzyme Q10 supplementation for the reduction of oxidative stress: clinical implications in the treatment of chronic diseases. International Journal of Molecular Sciences 21:7870. PMID: https://pubmed.ncbi.nlm.nih.gov/33114148
- Kumar A, Kaur H, Devi P, Mohan V (2009) Role of coenzyme Q10 (CoQ10) in cardiac disease, hypertension and Meniere-like syndrome. Pharmacology & Therapeutics 124:259-268. PMID: https://pubmed.ncbi.nlm.nih.gov/19638284
- Coppadoro A, Berra L, Kumar A et al. (2013) Critical illness is associated with decreased plasma levels of coenzyme Q10: a cross-sectional study. Journal of Critical Care 28:571-576. PMID: https://pubmed.ncbi.nlm.nih.gov/23618779
- Soltani R, Alikiaie B, Shafiee F et al. (2020) Coenzyme Q10 improves the survival and reduces inflammatory markers in septic patients. Bratislavske Lekarske Listy 121:154-158. PMID: https://pubmed.ncbi.nlm.nih.gov/32115970
- Shimizu M, Miyazaki T, Takagi A et al. (2017) Low circulating coenzyme Q10 during acute phase is associated with inflammation, malnutrition, and in-hospital mortality in patients admitted to the coronary care unit. Heart Vessels 32:668-673. PMID: https://pubmed.ncbi.nlm.nih.gov/27942805
- Langsjoen P, Langsjoen J, Langsjoen A, Rosenfeldt R (2019) Statin-associated cardiomyopathy responds to statin withdrawal and administration of coenzyme Q10. The Permanente Journal 23:18. [257. PMID: https://pubmed.ncbi.nlm.nih.gov/31496499
- Zlatohlavek L, Vrablik M, Grauova B et al. (2012) The effect of coenzyme Q10 in statin myopathy. Neuro Endocrinology Letters 33 Suppl 2:98-101. PMID: https://pubmed.ncbi.nlm.nih.gov/23183519
- Qu J, Kaufman Y, Washington I (2009) Coenzyme Q10 in the human retina. Investigative Ophthalmology & Visual Science 50:1814-1818. PMID: https://pubmed.ncbi.nlm.nih.gov/19060288
- Aaseth J, Alexander J, Alehagen (2021) Coenzyme Q10 supplementation-in ageing and disease. Mechanisms of Ageing and Development 197:111521. PMID: https://pubmed.ncbi.nlm.nih.gov/34129891
- Kalen A, Appelkvist E, Dallner G (1989) Age-related changes in the lipid compositions of rat and human tissues. Lipids 24:579-584. PMID: https://pubmed.ncbi.nlm.nih.gov/2779364
- Acosta M, Fonseca L, Desbats M et al. (2016) Coenzyme Q10 biosynthesis in health and disease. Biochimica et Biophysica Acta 1857:1079-1085. PMID: https://pubmed.ncbi.nlm.nih.gov/27060254
- Schwemmlein J, Maack C, Bertero E (2022) Mitochondria as therapeutic targets in heart failure. Current Heart Failure Reports 19:27-37. PMID: https://pubmed.ncbi.nlm.nih.gov/35147851
- Starling R, Hammer D, Altschuld R (1998) Human myocardial ATP content and in vivo contractile function. Molecular and Cellular Biochemistry 180:171-177. PMID: https://pubmed.ncbi.nlm.nih.gov/9546644
- Bays H, Rader D (2009) Does nicotinic acid (niacin) lower blood pressure? International Journal of Clinical Practice 63:151-159. PMID: https://pubmed.ncbi.nlm.nih.gov/19054161
- Trueblood N, Ramasamy R, Wang L, Schaefer S (2000) Niacin protects the isolated heart from ischemia-reperfusion injury. American Journal of Physiology: Heart and Circulatory Physiology 279:H764-H771. PMID: https://pubmed.ncbi.nlm.nih.gov/10924076
- Diguet N, Trammell S, Tannous C et al. (2018) Nicotinamide riboside preserves cardiac function in a mouse model of dilated cardiomyopathy. Circulation 137:2256-2273. PMID: https://pubmed.ncbi.nlm.nih.gov/29217642
- Rotllan N, Camacho M, Tondo M et al. (2021) Therapeutic potential of emerging NAD+-increasing strategies for cardiovascular diseases. Antioxidants 10:1939. PMID: https://pubmed.ncbi.nlm.nih.gov/34943043
- Tannous C, Booz G, Altara R et al. (2021) Nicotinamide adenine dinucleotide: biosynthesis, consumption and therapeutic role in cardiac diseases. Acta Physiologica 231:e13551. PMD: https://pubmed.ncbi.nlm.nih.gov/32853469
- Abdellatif M, Trummer-Herbst V, Koser F et al. (2021) Nicotinamide for the treatment of heart failure with preserved ejection fraction. Science Translational Medicine 13:eabd7064. PMID: https://pubmed.ncbi.nlm.nih.gov/33568522
- Abdellatif M, Sedej S, Kroemer G (2021) NAD+ metabolism in cardiac health, aging, and disease. Circulation 144:1795-1817. PMID: https://pubmed.ncbi.nlm.nih.gov/34843394
- Vignier N, Chatzifrangkeskou M, Rodriguez B et al. (2018) Rescue of biosynthesis of nicotinamide adenine dinucleotide protects the heart in cardiomyopathy caused by lamin A/C gene mutation. Human Molecular Genetics 27:3870-3880. PMID: https://pubmed.ncbi.nlm.nih.gov/30053027
- Podyacheva E, Yu N, Vsevolod V et al. (2022) Intravenous nicotinamide riboside administration has a cardioprotective effect in chronic doxorubicin-induced cardiomyopathy. International Journal of Molecular Sciences 23:13096. PMID: https://pubmed.ncbi.nlm.nih.gov/36361882
- Tong D, Schiattarella G, Jiang N et al. (2021) NAD+ repletion reverses heart failure with preserved ejection fraction. Circulation Research 128:1629-1641. PMID: https://pubmed.ncbi.nlm.nih.gov/33882692
- Zhu X, Li J, Wang H et al. (2023) Nicotinamide restores tissue NAD+ and improves survival in rodent models of cardiac arrest. PLoS One 18:e0291598. PMID: https://pubmed.ncbi.nlm.nih.gov/37713442
- Levy T (2023) https://www.tomlevymd.com/articles/omns20231012/Schizophrenia-Is-Chronic-Encephalitis...and-Niacin-Cures-It
- Holubiec P, Lenoczyk M, Staszewski F et al. (2021) Pathophysiology and clinical management of pellagra-a review. Folia Medica Cracoviensia 61:125-137. PMID: https://pubmed.ncbi.nlm.nih.gov/34882669
- Rivadeneira A, Moyer P, Salciccioli J (2019) Pellagra in the USA: unusual manifestations of a rare entity. BMJ Case Reports 12:e230972. PMID: https://pubmed.ncbi.nlm.nih.gov/31570356
- Seftel H (1972) Cardiomyopathies in Johannesburg Bantu. II. Aetiology of idiopathic cardiomyopathy. South African Medical Journal 46:1823-1828. PMID: https://pubmed.ncbi.nlm.nih.gov/4649262
- Schwartz B, Gjini P, Gopal D, Fetterman J (2022) Inefficient batteries in heart failure: metabolic bottlenecks disrupting the mitochondrial ecosystem. JACC: Basic to Translational Science 7:1161-1179. PMID: https://pubmed.ncbi.nlm.nih.gov/36687274
- Wang G, Li W, Lu X, Zhao X (2011) Riboflavin alleviates cardiac failure in type I diabetic cardiomyopathy. Heart International 6:e21. PMID: https://pubmed.ncbi.nlm.nih.gov/22355488
- Kotegawa M, Sugiyama M, Haramaki N (1994) Protective effects of riboflavin and its derivatives against ischemic reperfused damage of rat heart. Biochemistry and Molecular Biology International 34:685-691. PMID: https://pubmed.ncbi.nlm.nih.gov/7866293
- Jain-Ghai S, Cameron J, Maawali A et al. (2013) Complex II deficiency-a case report and review of the literature. American Journal of Medical Genetics: Part A 161A:285-294. PMID: https://pubmed.ncbi.nlm.nih.gov/23322652
- Otto A, Stahle I, Klein R et al. (1998) Anti-mitochondrial antibodies in patients with dilated cardiomyopathy (anti-M7) are directed against flavoenzymes with covalently bound FAD. Clinical and Experimental Immunology 111:541-547. PMID: https://pubmed.ncbi.nlm.nih.gov/9528896
- Yang L, Youngblood H, Wu C, Zhang Q (2020) Mitochondria as a target for neuroprotection: role of methylene blue and photobiomodulation. Translational Neurodegeneration 9:19. PMID: https://pubmed.ncbi.nlm.nih.gov/32475349
- Lin A, Poteet E, Du F et al. (2012) Methylene blue as a cerebral metabolic and hemodynamic enhancer. PLoS One 7:e46585. PMID: https://pubmed.ncbi.nlm.nih.gov/23056355
- Tretter I, Horvath G, Holgyesi A et al. (2014) Enhanced hydrogen peroxide generation accompanies the beneficial bioenergetic effects of methylene blue in isolated brain mitochondria. Free Radical Biology & Medicine 77:317-330. PMID: https://pubmed.ncbi.nlm.nih.gov/25277417
- Gonzalez-Lima F, Auchter A (2015) Protection against neurodegeneration with low-dose methylene blue and near-infrared light. Frontiers in Cellular Neuroscience 9:179. PMID: https://pubmed.ncbi.nlm.nih.gov/26029050
- Tucker D, Lu Y, Zhang Q (2018) From mitochondrial function to neuroprotection-an emerging role for methylene blue. Molecular Neurobiology 55:5137-5153. PMID: https://pubmed.ncbi.nlm.nih.gov/28840449
- Svab G, Kokas M, Sipos I et al. (2021) Methylene blue bridges the inhibition and produces unusual respiratory changes in complex III-inhibited mitochondria. Studies on rates, mice and guinea pigs. Antioxidants 10:305. PMID: https://pubmed.ncbi.nlm.nih.gov/33669457
- Xue H, Thaivalappil A, Cao K (2021) The potentials of methylene blue as an anti-aging drug. Cells 10:3379. PMID: https://pubmed.ncbi.nlm.nih.gov/34943887
- Atamna H, Kumar R (2010) Protective role of methylene blue in Alzheimer's diseases via mitochondria and cytochrome c oxidase. Journal of Alzheimer's Disease 2:S439-452. PMID: https://pubmed.ncbi.nlm.nih.gov/20463399
- Jaiswal A, Kumar M, Silver E (2020) Extended continuous infusion of methylene blue for refractory septic shock. Indian Journal of Critical Care Medicine 24:206-207. PMID: https://pubmed.ncbi.nlm.nih.gov/32435102
- Dumbarton T, Minor S, Yeung C, Green R (2011) Prolonged methylene blue infusion in refractory septic shock: a case report. Canadian Journal of Anaesthesia 58:401-405. PMID: https://pubmed.ncbi.nlm.nih.gov/21246318
- Schlesinger J, Burger C (2016) Methylene blue for acute septic cardiomyopathy in a burned patient. Journal of Burn Care & Research 37:e287-291. PMID: https://pubmed.ncbi.nlm.nih.gov/25798807
- Brown G, Frankl D, Phang T (1996) Continuous infusion of methylene blue for septic shock. Postgraduate Medical Journal 72:612-614. PMID: https://pubmed.ncbi.nlm.nih.gov/8977944
- Kirov M, Evgenov O, Evgenov N et al. (2001) Infusion of methylene blue in human septic shock: a pilot, randomized, controlled study. Critical Care Medicine 29:1860-1867. PMID: https://pubmed.ncbi.nlm.nih.gov/11588440
- Lo J, Darracq M, Clark R (2014) A review of methylene blue treatment for cardiovascular collapse. The Journal of Emergency Medicine 46:670-679. PMID: https://pubmed.ncbi.nlm.nih.gov/24508113
- Duicu O, Privistirescu A, Wolf A et al. (2017) Methylene blue improves mitochondrial respiration and decreases oxidative stress in a substrate-dependent manner in diabetic rat hearts. Canadian Journal of Physiology and Pharmacology 95:1376-1382. PMID: https://pubmed.ncbi.nlm.nih.gov/28738167
- Berthiaume J, Hsiung C, Austin A et al. (2017) Methylene blue decreases mitochondrial lysine acetylation in the diabetic rat heart. Molecular and Cellular Biochemistry 432:7-24. PMID: https://pubmed.ncbi.nlm.nih.gov/28303408
- Ruha A (2013) Recommendations for provoked challenge urine testing. Journal of Medical Toxicology 9:318-325. PMID: https://pubmed.ncbi.nlm.nih.gov/24113861
- Bengtson U, Hylander L (2017) Increased mercury emissions from modern dental amalgams. Biometals 30:277-283. PMID: https://pubmed.ncbi.nlm.nih.gov/28220332
- Edlich R, Greene J, Cochran A et al. (2007) Need for informed consent for dentists who use mercury amalgam restorative material as well as technical considerations in removal of dental amalgam restorations. Journal of Environmental Pathology, Toxicology and Oncology 26:305-322. PMID: https://pubmed.ncbi.nlm.nih.gov/18197828
- Siblerud R (1990) The relationship between mercury from dental amalgam and the cardiovascular system. The Science of the Total Environment 99:23-35. PMID: https://pubmed.ncbi.nlm.nih.gov/2270468
- Khordi-Mood M, Sarraf-Shirazi A, Balali-Mood M (2001) Urinary mercury excretion following amalgam filling in children. Journal of Toxicology: Clinical Toxicology 39:701-705. PMID: https://pubmed.ncbi.nlm.nih.gov/11778667
- Al-Ayadhi L (2005) Heavy metals and trace elements in hair samples of autistic children in central Saudi Arabia. Neurosciences 10:213-218. PMID: https://pubmed.ncbi.nlm.nih.gov/22473261
- Adams J, Baral M, Geis E et al. (2009) Safety and efficacy of oral DMSA therapy for children with autism spectrum disorders: Part A-medical results. BMC Clinical Pharmacology 9:16. PMID: https://pubmed.ncbi.nlm.nih.gov/19852789
- Periferakis A, Caruntu A, Periferakis A-T et al. (2022) Availability, toxicology and medical significance of antimony. International Journal of Environmental Research and Public Health 19:4669. PMID: https://pubmed.ncbi.nlm.nih.gov/35457536
- Yang Y, Genesi B, Adams A (2023) Collection tubes can cause false elevations in occupational and clinical evaluation of antimony exposure. Journal of Analytical Toxicology 46:1079-1083. PMID: https://pubmed.ncbi.nlm.nih.gov/35141746
- Iijima A, Sato K, Yano K et al. (2008) Emission factor for antimony in brake abrasion dusts as one of the most atmospheric antimony sources. Environmental Science & Technology 42:2937-2942. PMID: https://pubmed.ncbi.nlm.nih.gov/18497147
- Krachler M, Zheng J, Koerner R et al. (2005) Increasing atmospheric antimony contamination in the northern hemisphere: snow and ice evidence from Devon Island, Arctic Canada. Journal of Environmental Monitoring 7:1169-1176. PMID: https://pubmed.ncbi.nlm.nih.gov/16307068
- Filella M, Belzile N, Chen Y (2002) Antimony in the environment: a review focused on natural waters. I. Occurrence. Earth-Science Reviews 57:125-176.
- Blanusa M, Varnai V, Piasek M, Kostial K (2005) Chelators as antidotes of metal toxicity: therapeutic and experimental aspects. Current Medicinal Chemistry 12:2771-2794. PMID: https://pubmed.ncbi.nlm.nih.gov/16305472
- Basinger M, Jones M (1981) Structural requirements for chelate antidotal efficacy in acute antimony(III) intoxication. Research Communications in Chemical Pathology and Pharmacology 32:355-363. PMID: https://pubmed.ncbi.nlm.nih.gov/6264554
- Kosnett M (2013) The role of chelation in the treatment of arsenic and mercury poisoning. Journal of Medical Toxicology 9:347-354. PMID: https://pubmed.ncbi.nlm.nih.gov/24178900
- Dawn L, Whited L (2023) Dimercaprol Treasure Island, FL: StatPearls Publishing
- Vega A, Delgado N, Handford M (2022) Increasing heavy metal tolerance by the exogenous application of organic acids. International Journal of Molecular Sciences 23:5438. PMID: https://pubmed.ncbi.nlm.nih.gov/35628249
- Thinh N, Osanai Y, Adachi T et al. (2021) Removal of lead and other toxic metals in heavily contaminated soil using biodegradable chelators: GLDA, citric acid and ascorbic acid. Chemosphere 263:127912. PMID: https://pubmed.ncbi.nlm.nih.gov/33297011
- Ke X, Zhang F, Zhou Y et al. (2020) Removal of Cd, Pb, Zn, Cu in smelter soil by citric acid leaching. Chemosphere 255:126690. PMID: https://pubmed.ncbi.nlm.nih.gov/32387903
- Jean L, Bordas F, Gautier-Moussard C et al. (2008) Effect of citric acid and EDTA on chromium and nickel uptake and translocation by Datura innoxia. Environmental Pollution 153:555-563. PMID: https://pubmed.ncbi.nlm.nih.gov/18029071
- Banihani S, Bayachou M, Alzoubi K (2015) L-carnitine is a calcium chelator: a reason for its useful and toxic effects in biological systems. Journal of Basic and Clinical Physiology and Pharmacology 26:141-145. PMID: https://pubmed.ncbi.nlm.nih.gov/25046310
- Bjorklund G, Oliinyk P, Lysiuk R et al. (2020) Arsenic intoxication: general aspects and chelating agents. Archives of Toxicology 94:1879-1897. PMID: https://pubmed.ncbi.nlm.nih.gov/32388818
- Dolev N, Katz Z, Ludmer Z et al. (2020) Natural amino acids as potential chelators for soil remediation. Environmental Research 183:109140. PMID: https://pubmed.ncbi.nlm.nih.gov/31999998
- Khaw K, Bingham S, Welch A et al. (2001) Relation between plasma ascorbic acid and mortality in men and women in EPIC-Norfolk prospective study: a prospective population study. European Prospective Investigation into Cancer and Nutrition. Lancet 357:657-663. PMID: https://pubmed.ncbi.nlm.nih.gov/11247548
- Ford E, Zhao G, Tsai J, Li C (2011) Vitamin D and all-cause mortality among adults in USA: findings from the National Health and Nutrition Examination Survey Linked Mortality Study. International Journal of Epidemiology 40:998-1005. PMID: https://pubmed.ncbi.nlm.nih.gov/21266455
- Naesgaard P, De La Fuente R, Nilsen S et al. (2012) Serum 25(OH)D is a 2-year predictor of all-cause mortality, cardiac death and sudden cardiac death in chest pain patients from Northern Argentina. PLoS One 7:e43228. PMID: https://pubmed.ncbi.nlm.nih.gov/22970121
- Reffelmann T, Ittermann T, Dorr M et al. (2011) Low serum magnesium concentrations predict cardiovascular and all-cause mortality. Atherosclerosis 219:280-284. PMID: https://pubmed.ncbi.nlm.nih.gov/21703623
- Ferre S, Li X, Adams-Huet B et al. (2018) Association of serum magnesium with all-cause mortality in patients with and without chronic kidney disease in the Dallas Heart Study. Nephrology, Dialysis, Transplantation 33:1389-1396. PMID: https://pubmed.ncbi.nlm.nih.gov/29077944
- Zhang X, Xia J, Del Gobbo L et al. (2018) Serum magnesium concentrations and all-cause, cardiovascular, and cancer mortality among U.S. adults: results from the NHANES I Epidemiologic Follow-up Study. Clinical Nutrition 37:1541-1549. PMID: https://pubmed.ncbi.nlm.nih.gov/28890274
- Mills E, O'Neill L (2014) Succinate: a metabolic signal in inflammation. Trends in Cell Biology 24:313-320. PMID: https://pubmed.ncbi.nlm.nih.gov/24361092
- Ogura S, Maruyama K, Hagiya Y et al. (2011) The effect of 5-aminolevulinic acid on cytochrome c oxidase activity in mouse liver. BMC Research Notes 4:66. PMID: https://pubmed.ncbi.nlm.nih.gov/21414200
- Shoolingin-Jordan P, Al-Daihan S, Alexeev D et al. (2003) 5-aminolevulinic acid synthase: mechanism, mutations and medicine. Biochimica et Biophysica Acta 1647:361-366. PMID: https://pubmed.ncbi.nlm.nih.gov/12686158
- Pierce J, Shen Q, Mahoney D et al. (2022) Effects of ubiquinol and/or D-ribose in patients with heart failure with preserved ejection fraction. The American Journal of Cardiology 176:79-88. PMID: https://pubmed.ncbi.nlm.nih.gov/35644694
- Paulson D (1998) Carnitine deficiency-induced cardiomyopathy. Molecular and Cellular Biochemistry 180:33-41. PMID: https://pubmed.ncbi.nlm.nih.gov/9546628
- Owen L, Sunram-Lea S (2011) Metabolic agents that enhance ATP can improve cognitive functioning: a review of the evidence for glucose, oxygen, pyruvate, creatine, and L-carnitine. Nutrients 3:735-755. PMID: https://pubmed.ncbi.nlm.nih.gov/22254121
Nutritional Medicine is Orthomolecular Medicine
Orthomolecular medicine uses safe, effective nutritional therapy to fight illness. For more information: http://www.orthomolecular.org
Find a Doctor
To locate an orthomolecular physician near you: http://orthomolecular.org/resources/omns/v06n09.shtml
The peer-reviewed Orthomolecular Medicine News Service is a non-profit and non-commercial informational resource.
Editorial Review Board:
Albert G. B. Amoa, MB.Ch.B, Ph.D. (Ghana)
Seth Ayettey, M.B., Ch.B., Ph.D. (Ghana)
Ilyès Baghli, M.D. (Algeria)
Barry Breger, M.D. (Canada)
Ian Brighthope, MBBS, FACNEM (Australia)
Gilbert Henri Crussol, D.M.D. (Spain)
Carolyn Dean, M.D., N.D. (USA)
Ian Dettman, Ph.D. (Australia)
Susan R. Downs, M.D., M.P.H. (USA)
Ron Ehrlich, B.D.S. (Australia)
Hugo Galindo, M.D. (Colombia)
Gary S. Goldman, Ph.D. (USA)
William B. Grant, Ph.D. (USA)
Claus Hancke, MD, FACAM (Denmark)
Patrick Holford, BSc (United Kingdom)
Ron Hunninghake, M.D. (USA)
Bo H. Jonsson, M.D., Ph.D. (Sweden)
Dwight Kalita, Ph.D. (USA)
Felix I. D. Konotey-Ahulu, M.D., FRCP (Ghana)
Peter H. Lauda, M.D. (Austria)
Fabrice Leu, N.D., (Switzerland)
Alan Lien, Ph.D. (Taiwan)
Homer Lim, M.D. (Philippines)
Stuart Lindsey, Pharm.D. (USA)
Pedro Gonzalez Lombana, M.D., Ph.D. (Colombia)
Victor A. Marcial-Vega, M.D. (Puerto Rico)
Juan Manuel Martinez, M.D. (Colombia)
Mignonne Mary, M.D. (USA)
Joseph Mercola, D.O. (USA)
Jorge R. Miranda-Massari, Pharm.D. (Puerto Rico)
Karin Munsterhjelm-Ahumada, M.D. (Finland)
Sarah Myhill, MB, BS (United Kingdom)
Tahar Naili, M.D. (Algeria)
Zhiyong Peng, M.D. (China)
Isabella Akyinbah Quakyi, Ph.D. (Ghana)
Selvam Rengasamy, MBBS, FRCOG (Malaysia)
Jeffrey A. Ruterbusch, D.O. (USA)
Gert E. Schuitemaker, Ph.D. (Netherlands)
Thomas N. Seyfried, Ph.D. (USA)
Han Ping Shi, M.D., Ph.D. (China)
T.E. Gabriel Stewart, M.B.B.CH. (Ireland)
Jagan Nathan Vamanan, M.D. (India)
Andrew W. Saul, Ph.D. (USA), Editor-In-Chief
Associate Editor: Robert G. Smith, Ph.D. (USA)
Editor, Japanese Edition: Atsuo Yanagisawa, M.D., Ph.D. (Japan)
Editor, Chinese Edition: Richard Cheng, M.D., Ph.D. (USA)
Editor, Norwegian Edition: Dag Viljen Poleszynski, Ph.D. (Norway)
Editor, Arabic Edition: Moustafa Kamel, R.Ph, P.G.C.M (Egypt)
Editor, Korean Edition: Hyoungjoo Shin, M.D. (South Korea)
Editor, Spanish Edition: Sonia Rita Rial, PhD (Argentina)
Editor, German Edition: Bernhard Welker, M.D. (Germany)
Associate Editor, German Edition: Gerhard Dachtler, M.Eng. (Germany)
Assistant Editor: Michael Passwater (USA)
Contributing Editor: Thomas E. Levy, M.D., J.D. (USA)
Contributing Editor: Damien Downing, M.B.B.S., M.R.S.B. (United Kingdom)
Contributing Editor: W. Todd Penberthy, Ph.D. (USA)
Contributing Editor: Ken Walker, M.D. (Canada)
Contributing Editor: Michael J. Gonzalez, N.M.D., Ph.D. (Puerto Rico)
Technology Editor: Michael S. Stewart, B.Sc.C.S. (USA)
Associate Technology Editor: Robert C. Kennedy, M.S. (USA)
Legal Consultant: Jason M. Saul, JD (USA)
Comments and media contact: drsaul@doctoryourself.com OMNS welcomes but is unable to respond to individual reader emails. Reader comments become the property of OMNS and may or may not be used for publication.
Click here to see a web copy of this news release: https://orthomolecular.activehosted.com/p_v.php?l=1&c=299&m=298&s=c7ae1002d2f579a22c16a1b89c854212
Article also available at Orthomolecular Medicine News Service
OMNS free subscription link http://orthomolecular.org/subscribe.html
OMNS archive link http://orthomolecular.org/resources/omns/index.shtml
Comments:
-
No Article Comments available