Positive Health Online
Your Country

Menopause Nutrition for IBS and your Gut
listed in ibs, originally published in issue 283 - January 2023
Many women experience gut symptoms in midlife. Bloating, gas, discomfort around your middle, diarrhoea or constipation are all common gut problems. They may be labelled as IBS and often flare up in peri menopause and menopause.
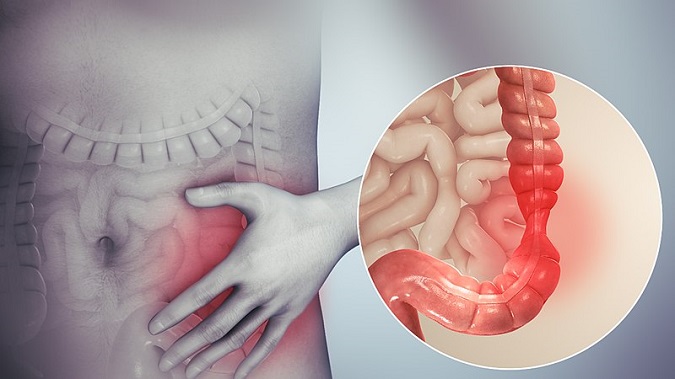
Irritable Bowel Syndrome
https://en.wikipedia.org/wiki/File:Irritable_bowel_syndrome.jpg
The Connection Between Menopause & Gut Symptoms
Whilst men can have gut symptoms too, they are more common in women.
Sex hormones, particularly oestrogen, have a powerful influence on the way your gut works. They do this by affecting the way your gut and brain communicate (known as the gut brain axis).
If you have experienced a flare up of IBS symptoms at certain times of your menstrual cycle, you will be very familiar with the effect your hormones have on your gut.[1]
There are several possible reasons why gut symptoms might flare up during the menopausal transition.
Poor Sleep
Lack of good quality sleep, a common occurrence in menopause, can lead to an imbalance in your nervous system. This in turn promotes increased inflammation that contributes to IBS symptoms.
Stress
Midlife can also be time of increased stress. Managing teenagers, looking after ageing parents, coming to terms with the loss of your fertile years and changes in your body’s appearance and functioning are some of the challenges faced by women in peri menopause.
When you are stressed or anxious, your brain sends messages to your gut which influence the way your intestines work.
Stress also affects the vital protective layer of cells in your gut known as your gut barrier. Keeping this barrier healthy is critical because it allows nutrients to be absorbed from the foods you eat but keeps harmful toxins out. If your gut barrier is not healthy, you are more likely to get IBS symptoms.[2]
Mood
Fluctuating hormone levels during peri menopause can affect your mood and make you feel demotivated. You may then be more likely to comfort eat and make unhelpful food choices. Junk food will be more prone to aggravate your gut symptoms. This creates an unhelpful cycle.
What Can You Do About It?
Feed Your Gut Microbiome
Your gut is home to trillions of bacteria, some beneficial and some not so. Keeping up the population of your good bacteria is key to a healthy gut environment. Research has recently found a link between the type of bacteria in your gut and your mood and mental health.[3]
If you are feeling better mentally, you may be less likely to over eat or binge on sugar rich foods that can play havoc with your gut.
How to Create Good Bacteria in Your Gut
The best way to do this is to eat plenty of soluble fibre. This type of fibre helps grow the good bacteria and crowd out the less desirable bacteria. Some types of fibre make IBS worse though so choose carefully.
Examples of helpful fibre are milled flaxseeds, wholegrains such as oats, brown rice, rye bread, quinoa and ground nuts.
You can also try fermented foods such as kefir or live yoghurt (try the dairy free versions of these foods if dairy affects your gut adversely).
Be Mindful of Trigger Foods
- Paying more attention to what you are eating will make a big difference to your gut. In your younger years you may have eaten a wide range of foods without them causing any gut issues. Unfortunately, the hormone fluctuations of the peri menopause can make your gut more sensitive and less resilient.
- Keep a food diary to see if you can pinpoint any trigger foods.
- Consulting a nutritional therapist can help you if you are getting confused about which foods are affecting you or feeling like you are cutting out too many foods. Overly restricted diets can lead to deficiencies of important nutrients.
- The FODMAP diet[4] has become well known recently. This diet cuts out many types of carbohydrates and in my opinion, unnecessary in most cases. In my nutrition practice, I avoid putting people on a full FODMAP diet because it is extremely restrictive and difficult to follow.
Exercise
Finally, look at exercise too. Regular exercise helps improve some symptoms of IBS, in particular bloating and constipation. Exercise helps the muscles of your large intestine to move food along it. It also increases muscle stimulation for bowel movements.[5]
Yoga has shown to be particularly effective for IBS symptoms in women.[6]
References
1.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4527267/Symptomatology of irritable bowel syndrome and inflammatory bowel disease during the menstrual cycle
2.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7925957/Intestinal barrier dysfunction in irritable bowel syndrome: a systematic review
3.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7213601/Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6089374/Brain structure and response to emotional stimuli as related to gut microbial profiles in healthy women
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4918736/Efficacy of the low FODMAP diet for treating irritable bowel syndrome: the evidence to date
5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4294172/Intervention to increase physical activity in irritable bowel syndrome shows long-term positive effects
6. https://www.Irritable Bowel Syndrome; Yoga as Remedial Therapy
Comments:
-
No Article Comments available