Positive Health Online
Your Country

Patients can do Much to Manage their Autoimmunity through Diet and Lifestyle Strategies
listed in immune function, originally published in issue 289 - September 2023
Autoimmune conditions represent a significant public health concern, affecting a substantial number of individuals globally. According to the American Autoimmune Related Diseases Association (AARDA), autoimmune diseases collectively impact more people than cancer[1] (9 million) and heart disease[2] (22 million) combined, affecting more than 50 million people in the US alone.[3] These are just the diagnosed cases; undiagnosed autoimmunity represents a significant concern given the difficulty in diagnosis.[4]
The good news is that patients can implement evidence-based strategies to optimize their potential to slow the progression of autoimmunity or put it into remission. I’ll review those basics in this article.
https://en.wikipedia.org/wiki/File:Fimmu-12-744396-g002.jpg
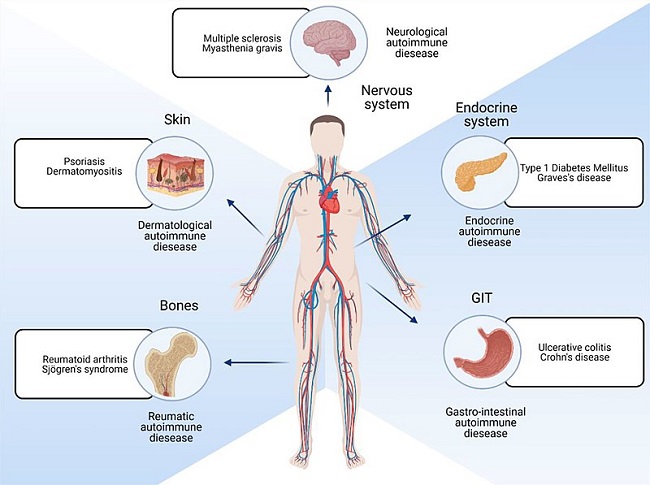
Different locations of the body that are affected by autoimmune diseases.
Credit: Katie Glover, Deepakkumar Mishra, and Thakur Raghu Raj Singh via Wikipedia
What is Autoimmunity?
Autoimmunity occurs when the immune system mistakenly attacks healthy cells in the body, leading to chronic inflammation and damage to various organs and tissues.[5] More than 80 different types of autoimmune diseases have been identified so far, including rheumatoid arthritis, lupus, multiple sclerosis, Hashimoto's thyroiditis, and celiac disease, to name just a few.[6]
Although autoimmune diseases can vary widely in their symptoms and severity, many significantly impact a person's quality of life. General symptoms can include chronic pain, fatigue, inflammation, depression, brain fog, organ damage, and overall functional impairment.[7]
Autoimmunity Frequently Overlooked in the Healthcare System
Unfortunately, healthcare providers frequently overlook or misdiagnose autoimmunity. Autoimmune reactions often present with a wide range of symptoms that may overlap with other conditions, making diagnosis challenging.[8] Additionally, there is a lack of education and awareness in the standard healthcare model around autoimmune disease diagnosis and clinical management.[9]
Approximately 75 percent of autoimmune patients are female. Research on medical gender disparity suggests this may contribute to underdiagnosis and undertreatment, as symptoms are often dismissed as hormonal or psychosomatic.[10]
The impact of misdiagnosis and underdiagnosis of autoimmunity cannot be underestimated. It leads to prolonged suffering, worsening of symptoms, and delayed access to appropriate treatment and support.
Managing Autoimmunity
Although it takes work on the patient’s part, many evidence-based resources such as books, websites, and courses exist to help educate patients. As autoimmune management, particularly in earlier stages, relies largely on diet and lifestyle modifications,[11] patients can implement these strategies to identify and address their underlying mechanisms or triggers.
It’s important to note that these strategies should not be seen as a replacement for necessary medication. For instance, when autoimmune Hashimoto’s has damaged enough of the thyroid gland, thyroid hormone replacement medication is necessary. However, implementing an autoimmune diet and lifestyle management plan can help slow or halt the progression of the disease and avoid increasing dosages of medication.
What Triggers Autoimmune Flareups
Symptoms of autoimmune disease depend on the tissue being affected. For instance, Hashimoto’s will produce low thyroid symptoms, rheumatoid arthritis will cause joint pain and deformity, and vitiligo will cause loss of skin pigmentation. Yet many autoimmune patients share common symptoms related to the chronic inflammation characteristic of unmanaged autoimmunity. These include chronic pain, fatigue, brain fog, muscle weakness, skin rashes, gastrointestinal issues, and recurring infections.[12]
A variety of factors can trigger autoimmune flare-ups, including:
- Stress: Emotional or physical stress can have a significant impact on the immune system and may trigger or exacerbate autoimmune symptoms.[13] Managing stress through techniques such as relaxation exercises, mindfulness, and therapy can be beneficial;[14]
- Infections: Viral or bacterial infections can stimulate the immune system and potentially trigger an autoimmune flare-up.[15] Many people have chronic undiagnosed viral, bacterial, fungal, or parasitic infections that may be promoting inflammation and autoimmune flares;
- Hormonal changes: Hormonal fluctuations, particularly in women during menstrual cycles, pregnancy, or menopause, can affect the immune system and lead to autoimmune flare-ups;[16]
- Pregnancy and postpartum: The immune system shifts dramatically during pregnancy and after childbirth. While these shifts are normal, for the person already predisposed to autoimmunity due to genetics, metabolic disorders, and chronic inflammation, pregnancy triggers autoimmunity in some women;[17]
- Diet and food sensitivities: Certain foods may trigger or worsen autoimmune symptoms in some individuals.[18] Common culprits include gluten, dairy, egg, soy, various grains, and food additives. We use the elimination-provocation diet or testing through Cyrex Labs to identify potential inflammatory foods;
- Environmental factors: Exposure to certain environmental triggers such as pollutants, chemicals, toxins, molds, or allergens can provoke autoimmune reactions.[19] Reducing exposure to triggers, improving indoor air quality, and adopting sustainable and toxin-free lifestyles can be beneficial.
Medications and treatments: Some medications, including certain antibiotics and nonsteroidal anti-inflammatory drugs (NSAIDs), can potentially trigger autoimmune flare-ups.[20] Additionally, certain medical treatments like radiation therapy or immunosuppressive drugs used to manage autoimmune diseases can have side effects that impact the immune system.
When comes to managing autoimmunity, a personalized approach is essential. Autoimmune diseases involve an overactive immune response that leads to chronic inflammation and damage to healthy tissues. Therefore, the goal of treatment is to dampen inflammation and modulate immune function.
Personalizing an Autoimmune Management Plan
Personalizing a management protocol for autoimmune diseases requires a multi-faceted approach.
If you look for autoimmunity resources with a functional medicine approach, you may be able to implement many management strategies yourself, which I introduce below.
Or consult with a functional medicine practitioner who specializes in autoimmune diseases. A qualified autoimmune specialist will be well-versed in common triggers of autoimmunity, appropriate lab testing, and evidence-based strategies to slow the progression or put it into remission.
Depending on the type and severity of your autoimmune disease, you may need a prescribing doctor to prescribe medications to manage symptoms, reduce inflammation, or suppress the immune system. This is especially true for cases where gland or organ function is compromised and you need replacement hormone medication, such as thyroid hormone.
The Importance of Identifying Inflammatory Triggers
It’s important is to identify potential triggers or factors that worsen your symptoms. These triggers vary from person to person and may include certain foods, environmental factors, or stressors. By identifying and avoiding these triggers, you may be able to better manage your symptoms.
Sometimes managing inflammatory triggers can be straightforward, such as eating an anti-inflammatory diet, reducing stress levels, getting regular exercise (but not over exercising), and prioritizing sleep;[21] These lifestyle modifications can help support overall immune function and reduce inflammation.
However, some autoimmune patients must make tough life choices when managing stress that provokes their symptoms. If you are in an abusive relationship, a toxic work situation, or in circumstances where you feel at a dead end and devoid of purpose, your health may require you make drastic lifestyle changes.
As cliché as it sounds, proven stress-reduction strategies such as yoga, meditation, tai chi, qi gong, and prayer can help. If early childhood trauma or past traumatic events keep you in a state of chronic stress, therapy can be a valuable part of your management strategy.
We can assess whether efforts to remove or mitigate inflammatory triggers is working through two means: assessing symptoms and lab markers.
If your efforts to dampen inflammation are working, you will start to feel better. Your symptoms will recede, and you’ll have more energy.
But you can also track inflammation using specific lab markers. Here are the lab markers and their optimal ranges that can help assess inflammation levels:
- C-reactive protein (CRP): Optimal range is 0-3. CRP is a marker of systemic inflammation, and elevated levels may indicate the presence of inflammation in the body.[22]
- Homocysteine: Optimal range is less than 8. Elevated homocysteine levels have been associated with increased inflammation and can be a risk factor for cardiovascular disease.[23]
- Ferritin: Pre-menopause range under 122; post-menopause range under 263; men range is under 236. Elevated ferritin levels can indicate inflammation or iron overload.[24]
- Lactate dehydrogenase (LDH): Optimal range is 140-180. LDH is an enzyme found in various tissues. High LDH levels may suggest tissue damage or inflammation,[25] and further testing can help identify the affected tissue.
- Uric acid: Women's range is 3.2-5.5; men's range is 3.7-6.0. Uric acid levels are associated with acute-phase reactants and can induce hepatic inflammatory molecules. Elevated uric acid levels may indicate inflammation.[26]
Monitoring these lab markers can provide valuable information about your inflammatory status. They should be decreasing on your autoimmune protocol.
Supplements that Support Autoimmunity
Supplements such as omega-3 fatty acids, vitamin D, liposomal glutathione, resveratrol, and curcumin have been studied for their potential benefits in supporting immune function and managing autoimmune conditions. While research is ongoing and individual responses may vary, these supplements have shown success in many of our clinic cases.
Research shows people who take vitamin D and omega 3 fatty acids are less likely to develop autoimmune disease. We find these compounds are essential in helping autoimmune patients manage their condition.[27
Over a 5-year period, those who took 2,000 IU of vitamin D a day either alone or in combination with 1 gram a day of omega 3s had a 30-40 percent lower rate of autoimmune disease development compared to those who took placebos.
Supplementation of omega 3 in combination with vitamin D was more effective than omega 3 alone.
Additionally, the more fat a person carries on their body the less vitamin D they appear to absorb.[28] Researchers theorize higher levels of body fat dilute vitamin D, a fat-soluble vitamin.
Omega-3 fatty acids, found in fatty fish like salmon and raw nuts, are known for their anti-inflammatory properties.[29] They may help regulate the immune response by reducing the production of inflammatory cytokines and promoting the production of anti-inflammatory molecules.
Most Westerners do not consume enough omega-3 fatty acids to support their heart, hormones, and brain.[30] I recommend that people managing their autoimmunity supplement with a sufficient amount of high-quality fish oil that is tested for purity. Research has shown that healthy dietary intake of omega-3 is 3500 mg for a person eating 2000 calories daily.
The average fish oil capsule contains only 1000 mg of omega-3 fats. That means if you eat 2000 calories a day (typical calorie intake in the United States is 2000 to 3000 calories a day) you should take 3 to 4 capsules of fish oil a day to support cardiovascular and brain health and reduce the risk of disease.
Adequate levels of vitamin D are important for immune health. Research suggests that vitamin D may help modulate immune responses, including those involved in autoimmune diseases. Some people with autoimmunity have a genetic polymorphism that inhibits uptake of D – they will need higher doses.[31] We may also give our overweight and obese patients higher doses.
Additionally, new research from Autoimmunity Research Foundation shows that the vitamin D receptors become downregulated by pathogens (such as parasites, bacteria, viruses, and yeast), compromising the uptake of vitamin D.[32]
It is recommended to maintain optimal vitamin D levels when you have autoimmunity. Test regularly to ensure optimal levels. The Vitamin D Council recommends the 25(OH)D test (and not the less accurate 1,25(OH)D).
Although traditional lab ranges for vitamin D are between 30 and 100 ng/ml, optimal levels are between 60 and 90 ng/ml, especially for those with an autoimmune condition. If your levels are below 60 ng/ml, I recommend taking between 5,000 to 10,000 UI of vitamin D per day and retesting after 3 to 4 months. Once your levels are above 60, you may be able to maintain them on 2,000 UI per day.
Another powerful nutraceutical is liposomal glutathione, our master antioxidant that helps protect cells from inflammatory damage. Many people are deficient in glutathione, particularly those with autoimmune diseases. Liposomal glutathione is a supplemental form that enhances absorption and has been shown to reduce inflammation and support immune function.[33] Your dose depends on your degree of inflammation, although I advise starting with a small dose to ensure you tolerate it.
A good complement to glutathione are liposomal turmeric and resveratrol, which are known for their antioxidant, immune regulating, and anti-inflammatory properties.[34] Again, you dose based on the degree of inflammation you are experiencing.
Managing autoimmunity is an ongoing process, and what works for one person may not work for another. It is important to develop a personalized management protocol that addresses your specific needs and goals and that evolves as you age or change life circumstances.
Monitoring your Antibody Levels
When living with an autoimmune disease, monitoring antibody levels is an important aspect of managing the condition. Antibodies are proteins produced by the immune system that target specific substances in the body, including healthy cells and tissues in the case of autoimmune diseases.
Regular monitoring of antibody levels can help establish a baseline and provide valuable information about the activity and progression of the autoimmune disease. It allows you to assess the effectiveness of your management strategies and lets your doctor know whether to make any necessary dosage adjustments in your medication.
The antibodies monitored will depend on the type of autoimmune disease being managed. For example, individuals with Hashimoto’s hypothyroidism must monitor their thyroid peroxidase (TPO) and thyroglobulin (Tg) antibodies.
Antibody tests are conducted through blood tests. I advise my patients to test their antibodies quarterly, particularly if they are changing their diet and lifestyle. Doing so will also allow you to establish your antibody baseline. Not everyone who achieves remission has antibodies in the normal lab range, and some with relatively low antibody counts can have heightened symptoms. This is due to an individual’s immune T and B cell function. What is more important is to monitor for deviations from your baseline.
Significant increases in antibody levels may indicate disease activity or a flare-up, while stable or decreasing levels may suggest that the treatment plan is effectively managing the condition.
It's important to note that antibody levels alone do not provide a complete picture of disease activity or symptom severity. Other factors, such as clinical symptoms and physical examinations, are also considered when assessing the overall management of an autoimmune disease.
Successful Autoimmune Management Depends on Patient Education and Empowerment
The standard healthcare model is designed to diagnose and treat autoimmune disease when it is in the end stages, significant tissue has been damaged, and medication is typically necessary. However, the autoimmune process begins years and even decades before things reach that degree of severity. During this time, patients suffer from ever-worsening symptoms, yet standard lab testing is normal. This is because screening for antibodies is not part of an annual exam.
By learning the basics of autoimmune symptoms and mechanisms and performing early screening, patients have the opportunity to implement evidence-based strategies that slow or halt the progression of their autoimmunity. Addressing inflammation and regulating immunity allows patients to live a more symptom-free life and lower the risk of developing subsequent autoimmune reactions and diseases.
References
- Jacques Ferlay et al., ‘Cancer Statistics for the Year 2020: An Overview’, International Journal of Cancer 149, no. 4 (15 August 2021): 778–89, https://doi.org/10.1002/ijc.33588 .
- Connie W. Tsao et al., ‘Heart Disease and Stroke Statistics—2022 Update: A Report From the American Heart Association’, Circulation 145, no. 8 (22 February 2022), https://doi.org/10.1161/CIR.0000000000001052 .
- Gregg E. Dinse et al., ‘Increasing Prevalence of Antinuclear Antibodies in the United States’, Arthritis & Rheumatology (Hoboken, N.J.) 72, no. 6 (June 2020): 1026–35, https://doi.org/10.1002/art.41214 .
- Frederick W Miller, ‘The Increasing Prevalence of Autoimmunity and Autoimmune Diseases: An Urgent Call to Action for Improved Understanding, Diagnosis, Treatment, and Prevention’, Current Opinion in Immunology 80 (February 2023): 102266, https://doi.org/10.1016/j.coi.2022.102266 .
- Philippa Marrack, John Kappler, and Brian L Kotzin, ‘Autoimmune Disease: Why and Where It Occurs’, Nature Medicine 7, no. 8 (2001): 899–905.
- Judy H Cho and Marc Feldman, ‘Heterogeneity of Autoimmune Diseases: Pathophysiologic Insights from Genetics and Implications for New Therapies’, Nature Medicine 21, no. 7 (July 2015): 730–38, https://doi.org/10.1038/nm.3897 .
- Dana K. Cassell and Noel R. Rose, The Encyclopedia of Autoimmune Diseases, The Facts On File Library of Health and Living (New York, N.Y: Facts On File, 2003).
- Cassell and Rose.
- Charlotte Lloyd et al., ‘Patient Priorities in Autoimmune Hepatitis: The Need for Better Treatments, More Education and Challenging Stigma’, Digestive Diseases and Sciences 68, no. 1 (January 2023): 87–97, https://doi.org/10.1007/s10620-022-07525-5 ; Melanie Sloan et al., ‘Medically Explained Symptoms: A Mixed Methods Study of Diagnostic, Symptom and Support Experiences of Patients with Lupus and Related Systemic Autoimmune Diseases’, Rheumatology Advances in Practice 4, no. 1 (1 January 2020): rkaa006, https://doi.org/10.1093/rap/rkaa006 .
- Fariha Angum et al., ‘The Prevalence of Autoimmune Disorders in Women: A Narrative Review’, Cureus, 13 May 2020, https://doi.org/10.7759/cureus.8094 .
- Edith Lahner et al., ‘Thyro-Entero-Gastric Autoimmunity: Pathophysiology and Implications for Patient Management’, Best Practice & Research Clinical Endocrinology & Metabolism 34, no. 1 (January 2020): 101373, https://doi.org/10.1016/j.beem.2019.101373 .
- Cassell and Rose, The Encyclopedia of Autoimmune Diseases.
- Ljudmila Stojanovich, ‘Stress and Autoimmunity’, Autoimmunity Reviews 9, no. 5 (March 2010): A271–76, https://doi.org/10.1016/j.autrev.2009.11.014 .
- Daniela Villani, Francesco Riva, and Giuseppe Riva, ‘New Technologies for Relaxation: The Role of Presence.’, International Journal of Stress Management 14, no. 3 (August 2007): 260–74, https://doi.org/10.1037/1072-5245.14.3.260 ; Clive J. Robins et al., ‘Effects of Mindfulness-Based Stress Reduction on Emotional Experience and Expression: A Randomized Controlled Trial’, Journal of Clinical Psychology 68, no. 1 (January 2012): 117–31, https://doi.org/10.1002/jclp.20857 .
- Shaye Kivity et al., ‘Infections and Autoimmunity – Friends or Foes?’, Trends in Immunology 30, no. 8 (August 2009): 409–14, https://doi.org/10.1016/j.it.2009.05.005 .
- Delia Almeida González et al., ‘Sex Hormones and Autoimmunity’, Immunology Letters 133, no. 1 (September 2010): 6–13, https://doi.org/10.1016/j.imlet.2010.07.001 .
- Yehuda Shoenfeld et al., ‘The Mosaic of Autoimmunity: Hormonal and Environmental Factors Involved in Autoimmune Diseases--2008’, The Israel Medical Association Journal 10, no. 1 (2008): 8.
- Arndt Manzel et al., ‘Role of “Western Diet” in Inflammatory Autoimmune Diseases’, Current Allergy and Asthma Reports 14, no. 1 (January 2014): 404, https://doi.org/10.1007/s11882-013-0404-6 .
- Chan-Na Zhao et al., ‘Emerging Role of Air Pollution in Autoimmune Diseases’, Autoimmunity Reviews 18, no. 6 (June 2019): 607–14, https://doi.org/10.1016/j.autrev.2018.12.010.
- Jean-François Bach, ‘Infections and Autoimmune Diseases’, Journal of Autoimmunity 25 (January 2005): 74–80, https://doi.org/10.1016/j.jaut.2005.09.024 .
- Manzel et al., ‘Role of “Western Diet” in Inflammatory Autoimmune Diseases’; Stojanovich, ‘Stress and Autoimmunity’; Peter Salmon, ‘Effects of Physical Exercise on Anxiety, Depression, and Sensitivity to Stress’, Clinical Psychology Review 21, no. 1 (February 2001): 33–61, https://doi.org/10.1016/S0272-7358(99)00032-X ; Valerie L. Jentsch and Oliver T. Wolf, ‘Acute Physical Exercise Promotes the Consolidation of Emotional Material’, Neurobiology of Learning and Memory 173 (September 2020): 107252, https://doi.org/10.1016/j.nlm.2020.107252 ; M Irwin, ‘Effects of Sleep and Sleep Loss on Immunity and Cytokines’, Brain, Behavior, and Immunity 16, no. 5 (October 2002): 503–12, https://doi.org/10.1016/S0889-1591(02)00003-X .
- Sara M. Nehring, Amandeep Goyal, and Bhupendra C. Patel, ‘C Reactive Protein’, in StatPearls (Treasure Island (FL): StatPearls Publishing, 2023), http://www.ncbi.nlm.nih.gov/books/NBK441843/ .
- Killian Robinson, ed., Homocysteine and Vascular Disease, vol. 230, Developments in Cardiovascular Medicine (Dordrecht: Springer Netherlands, 2000), https://doi.org/10.1007/978-94-017-1789-2 .
- Douglas B. Kell and Etheresia Pretorius, ‘Serum Ferritin Is an Important Inflammatory Disease Marker, as It Is Mainly a Leakage Product from Damaged Cells’, Metallomics 6, no. 4 (2014): 748–73, https://doi.org/10.1039/C3MT00347G .
- M Drent et al., ‘Usefulness of Lactate Dehydrogenase and Its Isoenzymes as Indicators of Lung Damage or Inflammation’, European Respiratory Journal 9, no. 8 (1996): 1736–42.
- Carmelinda Ruggiero et al., ‘Uric Acid and Inflammatory Markers’, European Heart Journal 27, no. 10 (1 May 2006): 1174–81, https://doi.org/10.1093/eurheartj/ehi879 .
- Jill Hahn et al., ‘Vitamin D and Marine Omega 3 Fatty Acid Supplementation and Incident Autoimmune Disease: VITAL Randomized Controlled Trial’, BMJ, 26 January 2022, e066452, https://doi.org/10.1136/bmj-2021-066452 .
- Vaibhav Kumar Maurya and Manjeet Aggarwal, ‘Factors Influencing the Absorption of Vitamin D in GIT: An Overview’, Journal of Food Science and Technology 54, no. 12 (November 2017): 3753–65, https://doi.org/10.1007/s13197-017-2840-0 .
- Artemis P. Simopoulos, ‘Omega-3 Fatty Acids in Inflammation and Autoimmune Diseases’, Journal of the American College of Nutrition 21, no. 6 (December 2002): 495–505, https://doi.org/10.1080/07315724.2002.10719248 .
- Artemis P Simopoulos, ‘The Importance of the Ratio of Omega-6/Omega-3 Essential Fatty Acids’, Biomedicine & Pharmacotherapy 56, no. 8 (2002): 365–79.
- Elias E. Mazokopakis et al., ‘Is Vitamin D Related to Pathogenesis and Treatment of Hashimoto’s Thyroiditis?’, Hellenic Journal of Nuclear Medicine 18, no. 3 (2015): 222–27.
- Paul J. Albert, Amy D. Proal, and Trevor G. Marshall, ‘Vitamin D: The Alternative Hypothesis’, Autoimmunity Reviews 8, no. 8 (July 2009): 639–44, https://doi.org/10.1016/j.autrev.2009.02.011 .
- Raghu Sinha et al., ‘Oral Supplementation with Liposomal Glutathione Elevates Body Stores of Glutathione and Markers of Immune Function’, European Journal of Clinical Nutrition 72, no. 1 (2018): 105–11.
- Shatadal Ghosh, Sharmistha Banerjee, and Parames C. Sil, ‘The Beneficial Role of Curcumin on Inflammation, Diabetes and Neurodegenerative Disease: A Recent Update’, Food and Chemical Toxicology 83 (September 2015): 111–24, https://doi.org/10.1016/j.fct.2015.05.022 ; Imogen Robertson et al., ‘The Science of Resveratrol, Formulation, Pharmacokinetic Barriers and Its Chemotherapeutic Potential’, International Journal of Pharmaceutics 618 (April 2022): 121605, https://doi.org/10.1016/j.ijpharm.2022.121605 .
Comments:
-
No Article Comments available