Positive Health Online
Your Country

Managing Fibromyalgia Requires Accurate Diagnosis and Addressing Mitochondrial Function
listed in fibromyalgia, originally published in issue 288 - August 2023
Fibromyalgia is a chronic condition affecting more than a million people in Australia that is characterized by widespread and diverse types of pain, including burning, stabbing, throbbing, and aching sensations. Patients also commonly report allodynia, when touch becomes painful, and nerve-associated pain such as numbness, tingling, and burning.
Other common symptoms include fatigue, post-exertional malaise, sleep problems, brain fog, poor brain function, muscle spasms, rashes, problems standing, irritable bowel symptoms, muscle weakness, myoclonic twitches, pelvic pain, poor coordination, and hypoglycemia.
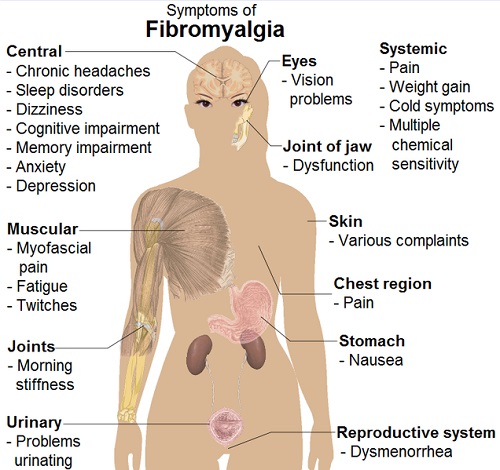
Common Signs and Symptoms of Fibromyalgia
Picture Credit: Mikael Häggström courtesy Wikipedia Commons
https://commons.wikimedia.org/wiki/File:Symptoms_of_fibromyalgia.png
Although it primarily affects young to middle-aged women, it can occur at any age and is also found in men.
Fibromyalgia can have multiple underlying causes, including:
- An increase in pain-producing pathways and a decrease in pain-inhibiting pathways.[1]
- Neurotransmitter imbalances, such as increased glutamate and reduced dopamine, serotonin, and opioid signaling in the brain.[2,3]]
- Central nervous system dysregulation.
- Brain inflammation.
- Chronic systemic inflammation.
- Damage to small nerve fibers may play a role.
- Autoimmunity
There is no consensus on what triggers fibromyalgia, and the exact cause is unknown. Researchers believe the condition may be due to changes in how the nervous system processes pain.[4]
The lack of correlation between fibromyalgia pain and joint problems has led many medical professionals to dismiss the condition as a psychological disorder.[5] However, studies show that fibromyalgia is primarily a central nervous system disorder that causes the brain to interpret normal stimuli as pain.
Make sure your Fibromyalgia Diagnosis isn’t Really Autoimmunity
Many patients with chronic symptoms that mimic fibromyalgia actually have an autoimmune disease. For instance, almost 40 percent of those with Hashimoto’s hypothyroidism, 30 percent with lupus, and 20 percent with rheumatoid arthritis have symptoms that mimic fibromyalgia.[5]
Other conditions misdiagnosed as fibromyalgia include other autoimmune diseases, neurological autoimmunity, chronic infections, Lyme disease, mold illness, and food and chemical intolerances.
As a result, patients never receive the proper help and treatment to alleviate their symptoms.
Fibromyalgia can be diagnosed by identifying pain in at least four body regions, with fatigue, sleep disturbances, and cognitive difficulties present for at least three months. Unfortunately, these can be symptoms of chronic inflammation and autoimmunity as well.
A qualified practitioner well versed in autoimmune and inflammatory disorders can untangle the cluster of symptoms and help patients with an appropriate care plan.
Managing Fibromyalgia Requires Improving Mitochondrial Health
Managing fibromyalgia is distinguished from chronic inflammatory disorders in that we must address the patient’s “bioenergetics,” or their energy metabolism. Chronic pain disorders often stem from a problem with a person’s energy production pathways.
Biopsy research suggests a link between fibromyalgia and mitochondrial abnormalities in muscle tissue.[6] This may explain why some patients with fibromyalgia experience constant muscle pain and aches.
Researchers also revealed that a disorder called the Warburg effect could lead to fibromyalgia. The Warburg effect increases lactate production and activates inflammatory pathways, leading to hyper pain sensitivity and inefficient muscle energy metabolism, particularly after exercise.
Strategies to Help Manage Fibromyalgia
Research has shown various strategies help manage fibromyalgia.[7]
Strategies include:
- A ketogenic diet (particularly in those suffering from the Warburg effect). Ketone bodies produced by a ketogenic diet have been found to reverse abnormal mitochondria function and reduce pain. A ketogenic diet also supports mitochondria by stabilizing blood sugar.[7]
- Improving sleep. REM sleep helps regulate mitochondrial biogenesis and maintenance and remove damaged mitochondria. Deep sleep helps repair and rejuvenate the mitochondria and regulate their metabolism.[8]
- Establishing a consistent circadian rhythm. Maintaining regular sleep patterns, exposure to natural light, and avoiding bright screens before bedtime can help support optimal mitochondrial function.[9.10,11]
- Anti-inflammatory supplements such as turmeric, curcumin, and glutathione can help address chronic pain.[12,13]
- CO Q-10. CO Q-10 helps alleviate pain, anxiety, brain activity associated with pain perception, mitochondrial oxidative stress, and inflammation in patients with fibromyalgia.[14]
The Importance of Physical Activity to Manage Fibromyalgia
Exercise is crucial in relieving fibromyalgia symptoms as it increases mitochondria in the muscles and organs.[15,16] This can help patients break out of the vicious cycle of chronic pain.
Some people’s issues with the Warburg effect or central nervous system dysfunctions may be too severe to exercise until they can better control them through the above-mentioned strategies. But for most patients, finding an exercise routine they can perform consistently is crucial. It initially takes trial, error, and motivation, but it's worth it in the long run. Regularly increasing heart rate and circulation turns on gene expressions that improve mitochondrial biogenesis, which increases energy levels while reducing chronic pain.
You don’t need to engage in high-intensity aerobic or strength training workouts. Instead, focus on activities you can perform daily that improve your metabolism and release endorphins and growth factors.
The goal is to work within your ability and to avoid “crashing” and worsening symptoms.
Examples include a 10-minute walk, gentle arm and leg movements, or riding a stationary bike. Starting with short workouts, gradually build up to longer and more intense routines, which will improve energy and reduce pain.
Ultimately, exercise is a critical component in reversing chronic pain. It improves mitochondrial function, circulation, inflammation, and immune modulation.
Available from Amazon.co.uk and Amazon.com
https://www.amazon.co.uk/Truth-About-Low-Thyroid-Hashimotos/dp/0976996219]
References
- Clauw DJ. Fibromyalgia and related conditions. Mayo Clin Proc. 2015 May;90(5):680-92. doi: 10.1016/j.mayocp.2015.03.014. PMID: 25939940.
- Murga I, Guillen V, Lafuente JV. Cerebral magnetic resonance changes associated with fibromyalgia syndrome. Med Clin (Barc). 2017 Jun 7;148(11):511-516. English, Spanish. doi: 10.1016/j.medcli.2017.01.034. Epub 2017 Apr 25. PMID: 28450073.
- Schwarz MJ, Späth M, Müller-Bardorff H, Pongratz DE, Bondy B, Ackenheil M. Relationship of substance P, 5-hydroxyindole acetic acid and tryptophan in serum of fibromyalgia patients. Neurosci Lett. 1999 Jan 15;259(3):196-8. doi: 10.1016/s0304-3940(98)00937-9. PMID: 10025591.
- https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Fibromyalgia https://rheumatology.org/patients/fibromyalgia
- Yunus MB, Kalyan-Raman UP, Masi AT, Aldag JC. Electron microscopic studies of muscle biopsy in primary fibromyalgia syndrome: a controlled and blinded study. J Rheumatol. 1989 Jan;16(1):97-101. PMID: 2716012.
- Sui BD, Xu TQ, Liu JW, Wei W, Zheng CX, Guo BL, Wang YY, Yang YL. Understanding the role of mitochondria in the pathogenesis of chronic pain. Postgrad Med J. 2013 Dec;89(1058):709-14. doi: 10.1136/postgradmedj-2012-131068. Epub 2013 Oct 22. PMID: 24151337.
- Castro-Marrero, J., Cordero, M.D., Segundo, M.J., et al. (2018). Could mitochondrial dysfunction be a differentiating marker between chronic fatigue syndrome and fibromyalgia? Antioxidants & Redox Signaling, 28(9), 757-761. doi: 10.1089/ars.2017.7316
- Melhuish Beaupre LM, Brown GM, Braganza NA, Kennedy JL, Gonçalves VF. Mitochondria's role in sleep: Novel insights from sleep deprivation and restriction studies. World J Biol Psychiatry. 2022 Jan;23(1):1-13. doi: 10.1080/15622975.2021.1907723. Epub 2021 May 6. PMID: 33821750.
- Bass, J., & Takahashi, J. S. (2010). Circadian integration of metabolism and energetics. Science, 330(6009), 1349-1354
- Vollmers, C., Gill, S., DiTacchio, L., Pulivarthy, S. R., Le, H. D., & Panda, S. (2009). Time of feeding and the intrinsic circadian clock drive rhythms in hepatic gene expression. Proceedings of the National Academy of Sciences, 106(50), 21453-21458.
- Eckel-Mahan, K. L., Patel, V. R., Mohney, R. P., Vignola, K. S., Baldi, P., & Sassone-Corsi, P. (2012). Coordination of the transcriptome and metabolome by the circadian clock. Proceedings of the National Academy of Sciences, 109(14), 5541-5546.
- Daily JW, Yang M, Kim DS, Park S. Efficacy of Turmeric Extracts and Curcumin for Alleviating the Symptoms of Joint Arthritis: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J Med Food. 2016 Aug;19(8):717-29.
- Ghezzi P, Jaquet V, Marcucci F, Schmidt H. The oxidative stress theory of disease: levels of evidence and epistemological aspects. Br J Pharmacol. 2018;175(12):1783-1796.
- Sawaddiruk P, Apaijai N, Paiboonworachat S, Kaewchur T, Kasitanon N, Jaiwongkam T, Kerdphoo S, Chattipakorn N, Chattipakorn SC. Coenzyme Q10 supplementation alleviates pain in pregabalin-treated fibromyalgia patients viareducing brain activity and mitochondrial dysfunction. Free Radic Res. 2019 Aug;53(8):901-909. doi: 10.1080/10715762.2019.1645955. Epub 2019 Aug 7. PMID: 31387429.
- Busch, A. J., Barber, K. A., Overend, T. J., Peloso, P. M., & Schachter, C. L. (2007). Exercise for treating fibromyalgia syndrome. Cochrane Database of Systematic Reviews, (4).
- Memme JM, Erlich AT, Phukan G, Hood DA. Exercise and mitochondrial health. J Physiol. 2021 Feb;599(3):803-817.
Comments:
-
No Article Comments available