Positive Health Online
Your Country

Advancements in Rectal Cancer Treatment: Enhancing and Improving Lives
by Dr Sandeep Nayak(more info)
listed in cancer, originally published in issue 290 - November 2023
Introduction
Rectal cancer is a type of colorectal cancer that affects the last part of the large intestine (colon). It is one of the most common cancers worldwide, with an estimated 43,340 new cases and 16,010 deaths in the United States in 2020. Rectal cancer can cause symptoms such as bleeding, pain, change in bowel habits, and weight loss. The risk factors for rectal cancer include age, family history, inflammatory bowel disease, obesity, smoking, and diet.
Rectal cancer is not only a significant global health concern but also poses a substantial burden in countries like India. In India, the incidence and mortality rates of rectal cancer are also notable, with a considerable number of cases diagnosed each year. The prevalence of risk factors such as age, family history, inflammatory bowel disease, obesity, smoking, and diet contributes to the rising incidence of rectal cancer in the Indian population. Healthcare professionals, public health initiatives, and cancer hospitals in India must address this growing challenge by implementing preventive measures, raising awareness about risk factors and symptoms, and ensuring access to timely and comprehensive diagnostic and treatment services. By focusing on early detection, personalized treatment approaches, and ongoing research, efforts can be made to improve outcomes and reduce the impact of rectal cancer on individuals in India and other affected countries.
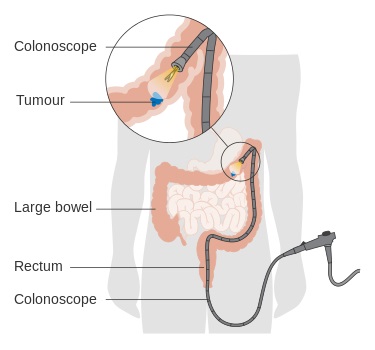
Diagram_showing_a_local_resection_of_an_early_stage_bowel_cancer
Credit: Wikipedia
The treatment of rectal cancer depends on the stage of the disease, the location and size of the tumor, and the patient's preferences and overall health. The main goals of treatment are to remove the cancer, prevent it from spreading or recurring, and preserve the function and quality of life of the patient. The main modalities of treatment are surgery, radiation therapy, and chemotherapy. In some cases, targeted therapies or immunotherapy may also be used.
Types of Treatments for Rectal Cancer
Surgery
Surgery is the primary treatment for rectal cancer. It involves removing the tumor along with a margin of healthy tissue and nearby lymph nodes. The type of surgery depends on the stage and location of the tumor.
- Early-stage cases: For tumours that are small and confined to the inner layer of the rectum, local excision or trans anal endoscopic microsurgery (TEM) may be performed. These procedures use special instruments to remove the tumour through the anus without making any incisions in the abdomen. They are less invasive and have fewer complications than other types of surgery;
- Advanced cases: For tumours that have grown deeper into the wall of the rectum or have spread to nearby lymph nodes or organs, partial or total mesorectal excision may be performed. These procedures involve removing part or all of the rectum along with surrounding fat and lymph nodes. They may be done through an open incision in the abdomen or by using a laparoscope (a thin tube with a camera and surgical tools) that is inserted through small cuts in the abdomen.
The importance of removing the tumour along with surrounding lymph nodes is to reduce the risk of recurrence and improve survival. The quality of surgery is measured by the completeness of mesorectal excision (CME), which means that no tumour cells are left behind in the mesorectum (the fat tissue around the rectum). Studies have shown that CME is associated with lower rates of local recurrence and better survival.
In some cases, surgery may require creating a temporary or permanent colostomy, which is an opening in the abdomen that allows stool to pass out of the body into a bag. This may be necessary if the tumour is too low in the rectum or if there is damage to the anal sphincter (the muscle that controls bowel movements). A colostomy can affect the patient's body image, self-esteem, and quality of life. However, there are ways to cope with a colostomy and live a normal life.
Radiation Therapy
Radiation therapy uses high-energy rays or particles to kill cancer cells or stop them from growing. It can be given before or after surgery for rectal cancer.
- Preoperative radiation therapy (neoadjuvant): This is given before surgery to shrink tumours and make them easier to remove. It may also reduce the risk of recurrence and improve survival. It is usually combined with chemotherapy (chemo radiation) for better results;
- Postoperative radiation therapy (adjuvant): This is given after surgery to eliminate any remaining cancer cells that may have been left behind or spread to nearby areas. It may also reduce the risk of recurrence and improve survival. It is usually combined with chemotherapy (chemo radiation) for better results.
There are two main types of radiation therapy for rectal cancer:
- External radiation therapy: This uses a machine that delivers high-energy X-ray beams to the tumour area from outside the body. The treatment is given in daily sessions for several weeks. The patient lies still on a table while a machine moves around them to deliver the radiation;
- Internal radiation therapy (brachytherapy): This uses radioactive sources that are placed inside or near the tumour through a catheter or applicator. The treatment is given in one or more sessions over a few days. The patient stays in the hospital while receiving this treatment;
- The side effects of radiation therapy depend on the dose, duration, and area treated. They may include fatigue, skin irritation, diarrhea, bladder problems, sexual dysfunction, infertility, and an increased risk of infection.
Chemotherapy
Chemotherapy uses drugs to target and kill cancer cells or stop them from growing. It can be given before, during, or after surgery for rectal cancer.
- Before surgery (neoadjuvant): This is given to shrink tumours and make them easier to remove. It may also reduce the risk of recurrence and improve survival. It is usually combined with radiation therapy (chemo radiation) for better results;
- During surgery (intraoperative): This is given directly into the blood vessels that supply blood to the tumor during surgery. It may increase the effectiveness of surgery by killing more cancer cells;
- After surgery (adjuvant): This is given to eliminate any remaining cancer cells that may have been left behind or spread to distant areas. It may also reduce the risk of recurrence and improve survival. It may be combined with radiation therapy (chemo radiation) for better results.
Chemotherapy can be administered in different ways:
- Intravenous: This means injecting the drugs into a vein through a needle or catheter;
- Oral: This means taking the drugs by mouth as pills or capsules.
The type and number of drugs used depend on the stage and characteristics of the tumour and the patient's preferences and overall health.
The common side effects of chemotherapy include nausea, vomiting, mouth sores, loss of appetite, hair loss, low blood cell counts, increased risk of infection, bleeding, bruising, fatigue, neuropathy, and allergic reactions.
Advancements in Treatment
Targeted Therapies
Targeted therapies are drugs that inhibit the growth and spread of cancer cells by targeting specific molecular alterations in the tumour. They are usually used in advanced cases or when cancer has spread to other parts of the body.
Some examples of targeted therapies for rectal cancer are:
- Anti-EGFR antibodies: These drugs block the epidermal growth factor receptor (EGFR), which is a protein that stimulates cell growth and division. They are used for tumours that do not have mutations in the KRAS gene, which makes them resistant to these drugs;
- Anti-VEGF antibodies: These drugs block the vascular endothelial growth factor (VEGF), which is a protein that stimulates blood vessel formation (angiogenesis). They are used to prevent tumours from getting oxygen and nutrients from new blood vessels;
- Anti-PD-1 antibodies: These drugs block the programmed cell death protein 1 (PD-1), which is a protein that inhibits the immune system from attacking cancer cells. They are used to enhance the immune system's ability to recognize and destroy cancer cells.
Targeted therapies are usually given in combination with chemotherapy for better results. They may cause side effects such as rash, diarrhea, high blood pressure, bleeding, infection, and liver problems.
Immunotherapy
Immunotherapy is a type of treatment that harnesses the body's immune system to recognize and destroy cancer cells. It is still being studied in clinical trials for rectal cancer and is not yet considered a standard treatment for all patients.
Some examples of immunotherapy for rectal cancer are:
- Checkpoint inhibitors: These drugs block proteins that prevent the immune system from attacking cancer cells. They are used for tumours that have high levels of microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR), which are genetic abnormalities that make them more visible to the immune system;
- Cancer vaccines: These drugs stimulate the immune system to produce antibodies against specific antigens on cancer cells. They are used to prevent recurrence or progression of disease after surgery or other treatments;
- Adoptive cell transfer: This technique involves collecting immune cells from the patient or a donor, modifying them in a laboratory to enhance their ability to fight cancer cells, and infusing them back into the patient. They are used to boost the immune system's response against tumours.
Immunotherapy may cause side effects such as inflammation, fever, fatigue, skin problems, endocrine disorders, and autoimmune reactions.
Conclusion
In conclusion, rectal cancer is a significant global health concern, and its impact is particularly notable in countries like India. The rising incidence and mortality rates of rectal cancer in India highlight the urgent need for preventive measures, awareness campaigns, and accessible diagnostic and treatment services. Healthcare professionals, public health initiatives, and cancer hospitals in India play a crucial role in addressing this challenge.
The main treatment modalities for rectal cancer include surgery, radiation therapy, and chemotherapy, to remove the tumour, prevent recurrence, and preserve the patient's quality of life. Advances in targeted therapies and immunotherapy offer additional options for patients with advanced or metastatic rectal cancer, holding promise for improved outcomes.
Personalized care, including tailored treatment plans and supportive measures, is essential to optimize treatment efficacy and manage treatment-related side effects. Close monitoring of patients and staying updated with the latest research allow oncologists to provide the best possible care.
Looking ahead, ongoing research and advancements in rectal cancer treatment offer hope for further improvements in outcomes. By combining scientific progress with compassionate care, healthcare professionals strive to reduce the burden of rectal cancer and enhance the lives of individuals affected by this disease. Continued efforts in prevention, early detection, and treatment will contribute to better outcomes and a brighter future for patients with rectal cancer.
Comments:
-
No Article Comments available