Positive Health Online
Your Country

The Causal Role of Autonomic Dysfunction and Lactic Acidosis in the Development of Diabetes Mellitus
by Carlos ETB Monteiro(more info)
listed in diabetes, originally published in issue 275 - January 2022
“With adrenalin a marked rise can occur, and instead of a fall in lactic acid we observed an actual rise amounting often to 100 percent. The results suggest that there is some factor common to the action both of insulin and adrenalin, which increases the lactic acid in spite of the divergent effects on the blood sugar” Tolstoi E, Loebel RO, Levine SZ and Richardson HB. 1924.[1]
Abstract
In the present article is postulated a new hypothesis that may explain the underlying causes of diabetes mellitus.
Some highlights:
- Diabetes is associated with overactive sympathetic nervous system what may lead to autonomic dysfunction;
- The autonomic dysfunction may accelerate glycolysis, what results in increased lactate production;
- Diabetes is associated with increased lactate production which gets worse the diabetic process;
- Obesity, an important risk factor for type 2 diabetes, is associated with autonomic dysfunction and high plasma lactate concentration;
- Type 2 diabetes is associated with increased cardiovascular mortality;
- The article shows potential drugs to fight diabetes by restoring the balance of the autonomic nervous system and reducing the production of lactic acid in the body.
Introduction
According to the World Health Organization (WHO) neither the cause of type 1 diabetes nor the means to prevent it are known.[2] Also, the sequence of events from the causal factors for both diabetes type 2 and gestational diabetes remain under discussion. As well it is unknown how to cure diabetes. Most people with diabetes have type 2.
The Pandemic of Diabetes
The number of people with diabetes rose from 108 million in 1980 to 422 million in 2014. About 8.5% of adults aged 18 years and older had diabetes in 2014. In 2019, diabetes was the direct cause of 1.5 million deaths. (WHO, 13 April 2021)
Autonomic Nervous System
The autonomic nervous system (ANS) is responsible for controlling many physiological functions: inducing the force of contraction of the heart, peripheral resistance of blood vessels and the heart rate. The ANS has both sympathetic and parasympathetic divisions that work together to maintain balance.
We support the concept that autonomic dysfunction is the precursor for the development of the diabetic mellitus process.
Autonomic Dysfunction in Diabetes
ANS also influences many of the functions of the body, including the pancreas. The parasympathetic nervous system (PNS) and the sympathetic nervous system (SNS) have opposing effects on insulin secretion from islet beta cells; feeding-induced parasympathetic neural activity to the pancreas stimulates insulin secretion, whereas stress-induced sympathetic neural activity to the pancreas inhibits insulin secretion.[3]
It has long been recognized that cardiac autonomic neuropathy (CAN) increases morbidity and mortality in diabetes and may have greater predictive power than traditional risk factors for cardiovascular events. This is attributable to the autonomic imbalance between the sympathetic and the parasympathetic nervous system regulation of cardiovascular function that is associated with both type 1 and type 2 diabetes.[4-7]
A study from 2001 have predicted: “As the world faces an obesity ‘epidemic, the mechanisms by which overweight is translated into insulin resistance, hypertension, and diabetes need to be better understood. Although the processes of transition remain uncertain, overactivity of the sympathetic nervous system appears pivotal”.[8]
A study from 2014[9] aimed to investigate the development of severe hypoglycemia (SH) in the presence of cardiovascular autonomic neuropathy (CAN) in patients with type 2 diabetes. A total of 894 patients with type 2 diabetes were enrolled. The authors found that in the long-term of the study (10 years), prospective, observational cohort study, was demonstrated a significant relationship between diabetic cardiovascular autonomic dysfunction and the development of SH in patients with type 2 diabetes during the follow-up period. They showed that a higher cardiovascular autonomic function test (AFT) score, especially a score indicating definite CAN, had a tendency to increase the risk of SH in patients with type 2 diabetes.
A study from 2019[10] aimed to determine clinical factors related to CAN recovery. It concluded that younger age is the most important factor in CAN recovery in subjects with type 2 diabetes, including recovery from the definite or severe stage. Glycated hemoglobin (HbA1c) reduction, body weight reduction, no concurrent micro/macro albuminuria, and shorter duration of diabetes were also significantly associated with CAN recovery. Another study, this one from 2021,[11] said that the poorer the glycaemic control and the longer the duration of the disease, the higher the incidence of CAN in T2DM and age, duration of disease, waist-hip ratio, and HbA1c, are well correlated with the severity of CAN.
The autonomic imbalance is also associated with gestational diabetes.[12]
The Association of Cardiovascular Disease (CVD) with Diabetes
Hypertension is common among patients with diabetes, with the prevalence depending on type and duration of diabetes, age, sex, race/ethnicity, BMI, history of glycemic control, and the presence of kidney disease, among other factors.[13] On the causal role for hypertension, involving the autonomic dysfunction and increased lactate production, see our recent article.[14]
A study from 2018 demonstrated that globally, overall cardiovascular disease affects approximately 32.2% of all persons with type 2 diabetes. CVD is a major cause of mortality among people with type 2 diabetes, accounting for approximately half of all deaths over the study period.[15]
Risk Factors for Diabetes Mellitus
Excess body weight and physical inactivity are foreseen as the most important factors for the development of type 2 diabetes. Obesity is believed to account for 80-85% of the risk of developing type 2 diabetes, while recent research suggests that obese people are up to 80 times more likely to develop type 2 diabetes than those with a BMI of less than 22.[16] Both obesity[17] and physical inactivity[18] are affected by autonomic dysfunction.
Recent studies have argued that added sugars increase the risk of obesity and diabetes. [19-22] The stimulatory effect of dietary carbohydrate on SNS activity was first recognized in 1977, during sucrose feeding.[23] Oral fructose has been shown to be as potent as glucose in stimulating the SNS in animals or human subjects.[24-26] Many studies have shown that high carbohydrate diets consumption may activate the sympathetic system.[27-30]
Exceptional glycemic control of type 1 diabetes with low rates of adverse events was reported in 2018 by a community of children and adults who consume a very low-carbohydrate diet.[31] The authors have highlighted in their paper:
“Before the discovery of insulin, the lives of children with type 1 diabetes mellitus were extended, sometimes for years, by severe carbohydrate restriction. After the advent of insulin treatment, the recommended carbohydrate intake was increased without clinical trial proof of superiority. By the 1980s, a low-fat diet containing up to 60% of energy from carbohydrates became the standard of care. More recently, the American Diabetes Association has emphasized the individualization of diet rather than focusing on macronutrients.”
Follows are some additional risk factors that may dysregulate the autonomic nervous system in diabetes type 2:
- Age[32,33]
- Tobacco[34]
A recent study demonstrated that elevated heart rate is independently, in interaction with a higher body mass index, associated with a higher incidence of type 2 diabetes mellitus.[35]
Resting electrocardiogram abnormalities are common in all people with type 2 diabetes, including those without a history of CVD; their prevalence is related to traditional cardiovascular risk factors such as older age, male sex, hypertension, lower HDL cholesterol, higher BMI, and smoking behavior.[36]
According to our present postulation the autonomic dysfunction leads to increased lactate production, which gets worse the diabetic disease process.
Increased Lactate Production in Diabetes
Diabetes can cause changes in the musculoskeletal system, which is the term for our muscles, bones, joints, ligaments, and tendons.[37] It is interesting to notice that, in 1874, Balthazar Foster found the administration of lactic acid by the mouth to diabetic patients resulted in painful and swollen joints. These manifestations persisted so long as the lactic acid was continued and disappeared when it was discontinued.[38]
Oswald Loeb, in a study from 1913,[39] was the first to link lactic acidosis to atherosclerosis. He has demonstrated in his experiments that injecting lactic acid to rabbits and dogs, resulted in atherosclerotic lesions in these animals. In his study he also mentioned about a similar hypothesis for diabetes, that follows:
“Let us remember that when we inject adrenaline and nicotine causes the most serious disturbances on the part of the animals blood pressure and breathing show, even temporarily, reactions with convulsions, so the assumption is not of that hard to indicate that it is a production or a less destruction of lactic acid. It is well known that rabbits react to adrenaline intake with glycosuria, it would not be impossible that with, simultaneous hyperglycemia, the build-up to sugar is disturbed and a greater build-up of lactic acid and thereby aldehyde formation would be given. We can also make a similar hypothesis for diabetes, in which is well known, arteriosclerosis occurs frequently. Remarkable is still that even those researchers who investigate arterial changes seen occurring with abnormal diet, report glycosuria and severe metabolic disorders.”
(Diabetes is also a risk factor for atherosclerosis under our acidity theory point of view. This theory was developed in 2006.[40])
A study from 1924[1] involved four patients with uncomplicated diabetes. They varied from extremely mild to moderately severe. In each case the effect of a single intravenous dose varying from 8 to 33 units of insulin (Iletin, Lilly) was observed. The blood was taken before, and between 1 and 2 hours after, the injection, and analyzed for sugar, lactic acid, and inorganic phosphates. The study has highlighted that
“With adrenalin a marked rise can occur, and instead of a fall in lactic acid we observed an actual rise amounting often to 100 percent. The results suggest that there is some factor common to the action both of insulin and adrenalin, which increases the lactic acid in spite of the divergent effects on the blood sugar.”
A comparison of the effects of insulin and adrenaline led the authors to the following conclusions:
- Both extracts lower the inorganic phosphate of the blood;
- Extreme drops in blood sugar may occur with no change in the lactic acid concentration. With our patients increases in lactic acid were observed only when an insulin hypoglycemia was produced, and this may turn out to be the general rule.
- Lactic acid increases with an adrenaline hyperglycemia;
- Insulin causes an increase in the respiratory quotient over and above that which can be accounted for by the production of lactic acid. This is evidence of the stimulating action exerted by the extract on the oxidation of carbohydrate.
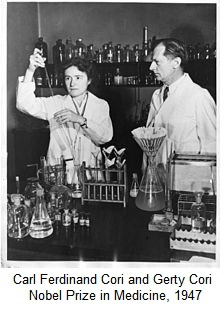
The above study was discussed in the same year by Carl Ferdinand Cori[41] who made experiences in animals in this direction, saying that his results and conclusions looked like to be in harmony with Tolstoi and colleagues’ findings.[1] Follows the results and conclusions from Cori:
- Insulin hypoglycemia produces no definite change in the lactic acid content of the blood of either fasting rabbits or cats, nor does insulin have an effect on the blood lactic acid of phlorhizinized rabbits or depancreatized cats;
- Insulin convulsions lead to a strong increase in the lactic acid concentration of the blood;
- Epinephrine causes a rise in the blood lactic acid of rabbits and cats. The effect is more marked in the former animals than in the latter;
- The lactic acid concentration in the liver and in the muscles of mice remained uninfluenced by insulin hypoglycemia, by insulin convulsions or coma plus convulsions, and by epinephrine. The free sugar content of the liver was strongly lowered by insulin and remained low in spite of insulin convulsions;
- It was concluded that insulin has no effect on the reaction glucose ⇄ lactic acid in the direction to the right.
A study from 1988[42] found that disturbed liver function and increased levels of lactate are early risk factors for diabetes.
The results of a study from 1990[43] suggested that even prior to frank carbohydrate intolerance, progressive changes in basal levels of glucose, insulin, and lactate, as well as sum of glucose, accompany the expansion of adipose mass in obesity. Two different aspects of lactate metabolism have been examined in obesity. First, the association of increased basal lactate levels with increased obesity may reflect increased lactate production from enlarged adipocytes and an increased fat mass. Secondly, the inverse association between acute lactate generation following glucose ingestion and obesity, despite the increased sum of glucose in obese subjects, may reflect a decreased ability of adipose and/or extra-adipose tissues to convert glucose to lactate due to insulin resistance.
A study from 1992 found that lactate is correlated with insulin resistance, independent of obesity.[44]
A study published in 1993[45] demonstrated that plasma lactate concentration was lowest in the non-obese group with normal glucose tolerance (0.81 +/- 0.07 mmol/L), highest in the obese subjects with type 2 diabetes (1.46 +/- 0.14 mmol/L), and intermediate in obese individuals with normal glucose tolerance (1.17 +/- 0.13 mmol/L).
A study from 2002 provided evidence that the elevation of plasma lactate suppressed glycolysis before its effect on insulin-stimulated glucose uptake, consistent with the hypothesis that suppression of glucose metabolism could precede and cause insulin resistance. In addition, lactate-induced insulin resistance was associated with impaired insulin signaling and decreased insulin-stimulated glucose transport in skeletal muscle.[46]
A study from 2007[47] concluded that adipose tissue (AT) and skeletal muscle (SM) are both significant sources of lactate release post-absorptivity, and AT is at least as responsive to insulin as SM. It was assumed by the authors that the ability to increase lactate release in response to insulin is impaired in AT and SM in insulin-resistant obese women, involving defective insulin regulation of both tissue lactate metabolism and local blood flow.
A study from 2010[48] confirmed that plasma lactate was strongly associated with type 2 diabetes in older adults. The authors said that plasma lactate deserves greater attention in studies of oxidative capacity and diabetes risk.
A study from 2015[49] suggested that an increase in lactate could herald the early stages of insulin resistance long time before patients are diagnosed with diabetes mellitus.
Another study from 2015,[50] postulated that elevated plasma lactate levels are part of the clinical spectrum of glycogenic hepatopathy in patients with poorly controlled type 1 diabetes.
A study from 2016[51] found that plasma lactate is independently associated with incident atrial fibrillation, and its contribution to AF may be, at least in part, mediated by diabetes and/or hypertension.
Sugars in excess may raise lactic acid production in the body.[52, 53]
Increased blood lactate concentration is also associated with gestational diabetes.[54]
How Autonomic Dysfunction Leads to Lactic Acidosis
The chronic elevated release of catecholamine precipitated by the sympathetic nervous system can accelerate glycolysis, which results in a significant increase in lactate production.
The influence of adrenaline on lactic acid production have been observed in the early 1920s by the Cori’s. They have discussed about this subject in 1929.[55] Carl Ferdinand Cori and his wife Gerty Cori received a Nobel Prize in1947 for their discovery of how glycogen – a derivative of glucose – is broken down and resynthesized in the body.
A 1982 article by David S Schade[56] provided further support for the direct participation of catecholamines in the development and/or maintenance of lactic acidosis as follows:
- The common association of stress and lactic acidosis;
- The rise in plasma lactate concentration during adrenaline infusion;
- The precipitation of lactic acidosis by adrenaline intoxication and pheochromocytoma;
- The vasoconstrictor effects of catecholamines leading to tissue anoxia and lactic acid production.
A study from John R. Williamson confirmed in 1964 the effects of adrenaline infusion on the increased production of lactate in isolated heart tissue, up to five times the normal production.[57]
The Controversial Use of Digitalis and Digitoxin in Diabetes Mellitus
In 1999,[58] a study reported three patients with type 2 diabetes mellitus who after digoxin, coincidentally discontinued, experienced better antidiabetic control with decreases in their blood glucose levels, making significant reductions in the antidiabetic treatment necessary.
Madsen in 2012, commented on a case report showing that patient’s levels of HbA1c and glucose rose significantly after commencement of digitoxin therapy. In his article[59] he told that “One thing that was learned was that the serum concentration should be lower than had been usual earlier”. Mentioning the study from 1999,[58] Madsen said that if there really is a connection between digitalis and exacerbated diabetes, it was very strange that this was not discovered earlier. He said that possible explanations are that the effects in most patients are less pronounced than in the present case, or that diabetes is so common among persons who take digitalis that exacerbation or a few extra cases are not noticed. He also told that, perhaps, more could be learned from looking at patients from the major blood pressure and heart failure studies who were given digitalis. He reasoned that in order to do this, access to original data would probably be necessary. Madsen also recommended that the HbA1c and glucose levels of patients with known diabetes be closely monitored after they start taking digitalis.
A study from 2016[60] found that digoxin reduced heart failure hospitalization in low ejection fraction patients with and without diabetes having no substantial risk of toxicity. It examined the efficacy and safety of digoxin in HF-REF patients with and without diabetes in the Digitalis Investigation Group trial (DIG). Mortality from all-cause, cardiovascular causes and heart failure (HF), along with HF hospitalization and suspected digoxin toxicity were analyzed according to diabetes status and randomized treatment assignment.
Of the 6800 patients, those with diabetes (n = 1933) were older, more often women, had worse clinical status and more co-morbidity than those without diabetes. All-cause and cardiovascular mortality were higher in patients with diabetes than in those without and digoxin did not reduce mortality in either sub-group. The rate of HF hospitalization (per 100 person-years) in patients with diabetes was higher than in those without and was reduced by digoxin in both patient groups: diabetes – placebo 20.5 and digoxin 16.0 (HR 0.79, 95% CI: 0.68–0.91); no diabetes – placebo 12.7 and digoxin 8.7 (HR 0.69, 0.62–0.77); interaction p = 0.14. Suspected digoxin toxicity in patients randomized to digoxin was more common among patients with diabetes than without (6.5% versus 5.8%), as was hospitalization for digoxin toxicity (1.4% versus 0.8%).
The patients were randomly assigned to receive digoxin or placebo. The initial dose of study drug was determined using an algorithm which took account of patient age, sex, weight, and renal function. The Investigators were permitted to modify dose of study drug based on other factors, such as use of concomitant drugs that might alter digoxin pharmacokinetics.
Overall, the daily dose of digoxin taken by the patients in this study was 0.125 mg in 17.5%, 0.250 mg in 70.6%, 0.375 mg in 10.3% and 0.500 mg in 1.1% of patients (median daily dose 0.250 mg). In patients with diabetes, the daily dose of digoxin taken was 0.125 mg in 17.5%, 0.250 mg in 69.1%, 0.375 mg in 12.7% and 0.500 mg in 0.8%. In patient without diabetes, the daily dose of digoxin taken was 0.125 mg in 20.3%, 0.250 mg in 69.5%, 0.375 mg in 9.0% and 0.500 mg in 1.1%. The median daily dose for patients with diabetes and those without was the same (0.250 mg).
According to this study[60] serum concentrations of digoxin were available only for a part of the study cohort, thus losing a great opportunity to compare patients, particularly diabetics, using lower digoxin concentration dosages versus those given higher concentration doses of this drug. This was taking into consideration the retrospective analysis of data by Rathore and col. in 2003[61] and Adams and col. in 2005,[62] of the DIG trial from 1997.[63] Their retrospective analysis has indicated a beneficial effect of digoxin on morbidity and no excess mortality at serum concentrations from 0.5 to 0.9 ng/ml, whereas serum concentrations > or =1.2 ng/ml seemed harmful.
These retrospective analyses of the DIG trial led the Heart Failure Society of America to issue new Heart Failure Guidelines in 2010.[64] Follow extracts of the Session 7 of these guidelines that are related to the use of Digoxin recommendations from the chapter Heart Failure in Patients with Reduced Ejection Fraction:
- Recent data suggest that the target dose (and serum concentration) of digoxin therapy should be lower than traditionally assumed. Although higher doses may be necessary for maximal hemodynamic effects, beneficial neurohormonal and functional effects appear to be achieved at relatively low serum digoxin concentrations (SDC) typically associated with daily doses of 0.125 to 0.25 mg. A retrospective analysis of the relationship of SDC to outcomes in the DIG trial demonstrated a strong direct relationship between the risk of death and SDC, with concentrations ≥ 1.2 ng/mL being associated with harm, whereas concentrations ≤ 1.0 ng/mL were associated with favorable outcomes;
- The efficacy of digoxin in HF with reduced Left Ventricular Ejection Fraction LVEF has traditionally been attributed to its relatively weak positive inotropic action arising from inhibition of sodium potassium ATPase and the resulting increase in cardiac myocyte intracellular calcium. However, digitalis has additional actions that may contribute significantly to its beneficial effects in patients with HF. Digoxin has important neuro-hormonal modulating effects that cannot be ascribed to its inotropic action, and it ameliorates autonomic dysfunction as shown by studies of heart rate variability, which indicate increased parasympathetic and baroreceptor sensitivity during therapy.
“Although there is not total agreement on the nature and clinical significance of the effects of digitalis on the autonomic nervous system, the following points seem well established and generally accepted: I) the actions of digitalis on the autonomic nervous system are very important clinically and play a major role in determining the clinical pharmacodynamic effects of the drug; 2) with therapeutic concentrations of the drug, the predominant effect is activation of vagal tone; and 3) with toxic concentrations of the drug there may be activation of sympathetic tone.” August M. Watanabe, 1985.[65]
Digoxin at Daily Low Concentration Dosages: The Magic Bullet to Fight Diabetes?
Digoxin and other cardiac glycosides, at low concentration dosages, can restore the balance of the autonomic nervous system and reduce the production of lactic acid in the body.
The Following Cardiac Glycosides Inhibit Sympathetic Overactivity:
- Cedilanid* [66]
- Digoxin [67,68]
- Digitoxin [69]
- Ouabain [70]
*Cedilanid is the trade name. The active ingredient is Lanatoside C
Cardiac Glycosides Reduce Lactate Production
A recent paper has demonstrated that inhibiting the overproduction of catecholamine by digoxin, digitoxin and ouabain may induce a potent inhibition of glycolysis (glucose consumption and lactate).[71] It confirms the results of old studies on this matter.[72]
ANS, Cardiac Glycosides, Hyperglycemia in Diabetes, and the Immune System
The results of many studies have established a critical role for the ANS in mediating interactions between the nervous and immune systems, two important adaptive systems that were originally considered to function independently of each other.[73]
Recently, a study has suggested that some cardiac glycosides activate immune responses.[74]
Hyperglycemia in diabetes may cause dysfunction of the immune response, which fails to control the spread of invading pathogens in diabetic subjects. Therefore, diabetic subjects are thought to be more susceptible to infections. The increased prevalence of type 2 diabetes will increase the incidence of infectious diseases and related comorbidities.[75]
Covid-19
It is important to cite the clinical perspective from a recent study showing that patients with cardiometabolic conditions, in particular obesity, hypertension, diabetes mellitus, and heart failure, have a high risk of poor outcomes from coronavirus disease 2019 infection. Among >900 000 US coronavirus disease 2019 hospitalizations through November 18, 2020, nearly two thirds (63.5%) were estimated to be attributable to these cardiometabolic conditions, that is, preventable if these conditions had not been present. The top risks were obesity (30.2%), hypertension (26.2%), and diabetes mellitus (20.5%).[76]
Incidentally, Covid-19 is associated with autonomic dysfunction[77] being the heart rate variability (HRV) associated with the severity of the disease.[78] The changing trend of HRV was related to the prognosis, indicating that HRV measurements can be used as a non-invasive predictor for clinical outcome of Covid-19. Also, elevated lactate levels were associated with poor prognosis in patients with Covid-19.[79]
A recent study[80] support cardiac glycosides with their electrophysiological and immunological properties merit a priority in the armor against COVID-19, especially when atrial arrhythmias complicate the in-hospital course.
Conclusion
The studies and concepts described in our present hypothesis provide strong evidence that autonomic dysfunction, as a precursor to the development of diabetes mellitus, being accompanied by increased lactic acid production, are important causal factors for this disease. The adoption of the directions proposed in the present article would open new horizons in the prevention of diabetes and in the search for new drugs, or the use of old drugs like cardiac glycosides. Therefore, offering the right solution in the prevention or in the treatment of diabetic patients.
References
- Tolstoi E, Loebel RO, Levine SZ and Richardson HB. The production of lactic acid in diabetes following the administration of insulin. Proceedings of the Society for Experimental Biology and Medicine, Volume 21, issue 8; page(s): 449-452 (1924) at https://journals.sagepub.com/doi/abs/10.3181/00379727-21-229?journalCode=ebma
- Diabetes: Key Facts. World Health Organization, June 8 (2020) at https://www.who.int/news-room/fact-sheets/detail/diabetes
- Kiba T. Relationships Between the Autonomic Nervous System and the Pancreas Including Regulation of Regeneration and Apoptosis. Pancreas 29:e51–e58 (2004) at https://pubmed.ncbi.nlm.nih.gov/15257115/
- Vinik AI, Mazer RE and Zieglert D. Autonomic imbalance: prophet of doom or scope for hope? Diabet. Med. 28, 643-651 (2011) at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3123705/
- Rosengård-Bärlund M, Bernardi L, Fagerudd J, Mäntysaari M et al. Early autonomic dysfunction in type 1 diabetes: a reversible disorder? Diabetologia volume 52, Article number 1164 (2009) at https://link.springer.com/article/10.1007/s00125-009-1340-9
- Weston PJ and Gill GV. Is undetected autonomic dysfunction responsible for sudden death in Type 1 diabetes mellitus? The ‘dead in bed’ syndrome revisited. Diabetic Medicine (2001) at https://onlinelibrary.wiley.com/doi/full/10.1046/j.1464-5491.1999.00121.x
- Carnethon MR, Jacobs DR Jr, Sidney S et al. Influence of Autonomic Nervous System Dysfunction on the Development of Type 2 Diabetes - The CARDIA study. Diabetes, 26(11): 3035-3041 (2003) at https://care.diabetesjournals.org/content/26/11/3035
- Esler M, Rumantir M, Wiesner G, Kaye D. Sympathetic nervous system and insulin resistance: from obesity to diabetes. Am J Hypertens. 14(11 Pt 2):304S-309S (2001) at https://pubmed.ncbi.nlm.nih.gov/11721888/
- Jae-Seung Yun, Ji-Hyun Kim, Ki-Ho Song, et al. Cardiovascular Autonomic Dysfunction Predicts Severe Hypoglycemia in Patients With Type 2 Diabetes: A 10-Year Follow-up Study. Diabetes Care Volume 37, (2014) at https://care.diabetesjournals.org/content/37/1/235
- Ji Eun Jun, Seung‑Eun Lee, Min Sun Choi, Sung Woon Park, You‑Cheol Hwang and Jae Hyeon Kim. Clinical factors associated with the recovery of cardiovascular autonomic neuropathy in patients with type 2 diabetes mellitus. Cardiovasc Diabetol 18:29 (2019) at https://cardiab.biomedcentral.com/articles/10.1186/s12933-019-0830-4
- Muhanad M. Dhumad, Farqad B. Hamdan, Mahmood S. Khudhair and Hisham Y. Correlation of staging and risk factors with cardiovascular autonomic neuropathy in patients with type II diabetes mellitus. Scientific Reports 11:3576 (2021) at https://www.nature.com/articles/s41598-021-80962-w
- Reyes LM, Khurana R, Usselman CW et al. Sympathetic nervous system activity and reactivity in women with gestational diabetes mellitus. Physiol Rep. 8(13): e14504 (2020) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7338594/
- de Boer IH, Bangalore S, Benetos A et al. Diabetes and Hypertension: A Position Statement by the American Diabetes Association. Diabetes Care, 40(9); 1273-1284 (2017) athttps://care.diabetesjournals.org/content/40/9/1273
- Monteiro CETB. The Causal Role of Autonomic Dysfunction and Lactic Acidosis in the Development ofhypertension. Positive Health Online Issue 271 (2021) at http://www.positivehealth.com/article/heart/the-causal-role-of-autonomic-dysfunction-and-lactic-acidosis-in-the-development-of-hypertension
- Einarson TR, Ludwig Craig and Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovascular Diabetology volume 17, Article number: 83 (2018) at https://cardiab.biomedcentral.com/articles/10.1186/s12933-018-0728-6
- co.uk. Diabetes and Obesity, 15th (2019) at https://www.diabetes.co.uk/diabetes-and-obesity.html
- Guarino D, Nannipieri M, Lervasi G et al. The Role of the Autonomic Nervous System in the Pathophysiology of Obesity. Front Physiol. 8, 665 (2017) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5606212
- Hughson RL and Shoemaker JK. Autonomic responses to exercise: deconditioning/inactivity. Auton Neurosci. 188:32-5 at (2015) https://pubmed.ncbi.nlm.nih.gov/25458429/
- Bray GA, Popkin BM. Dietary sugar and body weight: have we reached a crisis in the epidemic of obesity and diabetes? Health Be Damned! Pour on the Sugar. Diabetes Care, 37; 950–956 (2014) at https://care.diabetesjournals.org/content/37/4/950.long
- Lustig RH, Schmidt LA, Brindis CD . Public health: the toxic truth about sugar. Nature, 482; 27–29 (2012) at https://www.nature.com/articles/482027a
- Basu S, Yoffe P, Hills N, Lustig RH. The relationship of sugar to population-level diabetes prevalence: an econometric analysis of repeated cross-sectional data. PLoS One, 8; e57873 (2013) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3584048/
- Goran MI, Ulijaszek SJ, Ventura EE . High fructose corn syrup and diabetes prevalence: a global perspective. Glob Public Health, 8; 55–64 (2013) at https://www.tandfonline.com/doi/abs/10.1080/17441692.2012.736257?journalCode=rgph20
- Young JB, Landsberg L: Stimulation of the sympathetic nervous system during sucrose feeding. Nature, 269 :615 –617 (1977) at https://www.nature.com/articles/269615a0
- Walgren MC, Young JB, Kaufman LN, Landsberg L: The effects of various carbohydrates on sympathetic activity in heart and interscapular brown adipose tissue (IBAT) of the rat. Metabolism, 36 :585 –594 (1987) at https://pubmed.ncbi.nlm.nih.gov/3587017/
- Jansen RW, Penterman BJ, van Lier HJ, Hoefnagels WH: Blood pressure reduction after oral glucose loading and its relation to age, blood pressure and insulin. Am J Cardiol. 60; 1087 –1091 (1987) at https://pubmed.ncbi.nlm.nih.gov/3314457/
- Van Gaal L, Mertens I, Vansant G, De Leeuw I: Carbohydrate-induced thermogenesis in obese women: effect of insulin and catecholamines. J Endocrinol Invest. 22 ;109 –114 (1999) at https://link.springer.com/article/10.1007/BF03350889
- Tentolouris N, Tsigos C, Perea D, et al. Differential effects of high-fat and high-carbohydrate isoenergetic meals on cardiac autonomic nervous system activity in lean and obese women. Metabolism, 52(11):1426-32 (2003) at https://pubmed.ncbi.nlm.nih.gov/14624401/
- Kopp W. Chronically increased activity of the sympathetic nervous system: Our diet-related “evolutionary” inheritance. The Journal of Nutrition, Health and Aging, 13; pages 27–29 (2009) at https://link.springer.com/article/10.1007/s12603-009-0005-1
- Young JB, Weiss J and Boufath N. Effects of Dietary Monosaccharides on Sympathetic Nervous System Activity in Adipose Tissues of Male Rats. Diabetes, 53(5); 1271-1278 (2004) at https://diabetes.diabetesjournals.org/content/53/5/1271
- Li TSE and Anderson GH. Dietary carbohydrate and the nervous system. Nutrition Research, Volume 7, Issue 12; Pages 1329-1339 (1987) at https://www.sciencedirect.com/science/article/abs/pii/S0271531787800945
- Lennerz BS, Barton A, Bernstein RK et al. Management of Type 1 Diabetes with a very low-carbohydrate diet. Pediatrics 141 (6) e2017334 (2018) at https://pediatrics.aappublications.org/content/141/6/e20173349
- Esler M, Hastings J, Lambert G et al. The influence of aging on the human sympathetic nervous system and brain norepinephrine turnover. Am J Physiol Regul Integr Comp Physiol. 282(3); R909-16 (2002) at https://pubmed.ncbi.nlm.nih.gov/11832414/
- Balasubramanian P, Hall D and Subramanian M. Sympathetic nervous system as a target for aging and obesity-related cardiovascular diseases. GeroScience. 41(1): 13–24 (2019) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6423215/
- Niedermaier ON, Smith ML, Beightol LA et al. Influence of cigarette smoking on human autonomic function. Circulation, 88(2):562-71 (1993) at https://pubmed.ncbi.nlm.nih.gov/8339419/
- Xu C, Zhong J, Zhu H et al. Independent and interactive associations of heart rate and body mass index or blood pressure with type 2 diabetes mellitus incidence: A prospective cohort study. J Diabetes Investig. 10(4), 1068–1074 (2019) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6626957/
- Harms PP, van der Heijden AA, Rutters F et al for ESCAPE-NET. Prevalence of ECG abnormalities in people with type 2 diabetes: The Hoorn Diabetes Care System cohort. Journal of Diabetes and Its Complications Volume 35, Issue 2, 107810 (2021) at https://www.sciencedirect.com/science/article/pii/S1056872720306048
- Diabetes and Your Joints. Clinical Diabetes, 19(3): 136-136 (2001) at https://clinical.diabetesjournals.org/content/19/3/136
- Foster, B.: Clinical Medicine, London, J. and A. Churchill, Clinical Medicine: Lectures and Essays (Books google), p. 143 - 157 (1874) at https://bit.ly/3cDhKMR
- O. Ueber experimentelle Arterienveränderungen mit besonderer Berücksichtigung der Wirkung der Milchsäure auf Grund eigener Versuche. Dtsch Med Wochenschr 39(38): 1819-1822 (1913) at https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0028-1128737
- Monteiro CETB. Acidity Theory of Atherosclerosis -- History, Pathophysiology, Therapeutics and Risk Factors – A Mini Review. Positive Health Online, Edition 226 (2015) at http://www.positivehealth.com/article/heart/acidity-theory-of-atherosclerosis-history-pathophysiology-therapeutics-and-risk-factors-a-mini-revie
- Cori CF. The influence of insulin and epinephrine on the lactic acid content of blood and tissues. Presented before the American Society of Biological Chemists in Washington, D. C., December 1924, Published in JBC, V 63; Issue 2: Pages 253-268 (1925) at https://www.sciencedirect.com/science/article/pii/S002192581884995X
- Ohlson LO., Larsson B., Bjorntorp P., et al. Risk factors for Type 2 (non-insulin-dependent) diabetes mellitus. Thirteen and one-half years of follow-up of the participants in a study of Swedish men born in 1913. Diabetologia, 31(11):798–805 (1988) at https://pubmed.ncbi.nlm.nih.gov/3234634/
- Lovejoy J, Mellen B, and Digirolamo M, “Lactate generation following glucose ingestion: relation to obesity, carbohydrate tolerance and insulin sensitivity,” International Journal of Obesity, vol. 14, no. 10, pp. 843–855 (1990) at https://pubmed.ncbi.nlm.nih.gov/2269580/
- Lovejoy J, Newby FD, Gebhart SS, DiGirolamo M: Insulin resistance in obesity is associated with elevated basal lactate levels and diminished lactate appearance following intravenous glucose and insulin. Metabolism 41:22–27 (1992) at https://www.sciencedirect.com/science/article/abs/pii/002604959290185D
- Chen YD, Varasteh BB and G M Reaven GM. “Plasma lactate concentration in obesity and type 2 diabetes,” Diabete et Metabolisme, 19(4):348-354 (1993) at https://europepmc.org/article/med/8293860
- Choi CS, Kim Y-B, Lee FN, et al. Lactate induces insulin resistance in skeletal muscle by suppressing glycolysis and impairing insulin signaling. Am J Physiol Endocrinol Metab 283: E233–E240 (2002) at https://journals.physiology.org/doi/full/10.1152/ajpendo.00557.2001
- Qvisth V, Hagström-Toft E, Moberg E, Sjöberg S and Bolinder J, “Lactate release from adipose tissue and skeletal muscle in vivo: Defective insulin regulation in insulin-resistant obese women,” American Journal of Physiology—Endocrinology and Metabolism, vol. 292, no. 3, pp. E709–E714 (2007) at https://pubmed.ncbi.nlm.nih.gov/17077346/
- Crawford SO, Hoogeveen RC, Brancati FL et al. Association of blood lactate with type 2 diabetes: the Atherosclerosis Risk in Communities Carotid MRI Study. Int J Epidemiol. 39(6):1647-55 (2010) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2992628/
- Berhane F, Fite A, Daboul N et al., “Plasma lactate levels increase during hyperinsulinemic euglycemic clamp and oral glucose tolerance test,” Journal of Diabetes Research, Article ID 102054 (2015) at https://www.hindawi.com/journals/jdr/2015/102054/
- Brouwers J, Ham JC , Wisse E et al., “Elevated lactate levels in patients with poorly regulated type 1 diabetes and glycogenic hepatopathy: a new feature of mauriac syndrome,” Diabetes Care, vol. 38, no. 2, pp. e11–e12 (2015) at https://care.diabetesjournals.org/content/38/2/e11.long
- Misra S, Matsushita K, Sang Y et al Abstract P007: Association of Plasma Lactate with Incident Atrial Fibrillation in the ARIC Study. Circulation133:AP007 (2016) at https://www.ahajournals.org/doi/10.1161/circ.133.suppl_1.p007
- Edwards HT, Bensley EH, Dill DB and Carpenter TM. Human Respiratory Quotients in Relation to Alveolar Carbon Dioxide and Blood Lactic Acid After Ingestion of Glucose, Fructose, or Galactose. Journal of Nutrition Vol. 27 No. 3: 241-251 (1944) at https://academic.oup.com/jn/article-abstract/27/3/241/4725717?redirectedFrom=fulltext
- Hallfrisch J. Metabolic effects of dietary fructose. FASEB J, Vol 4; 2652-2660 (1990) at https://www.ncbi.nlm.nih.gov/pubmed/2189777
- Nagalakshmi CS, Santhosh NU, Krishnamurthy N et al. Role of Altered Venous Blood Lactate and HbA1c in Women with Gestational Diabetes Mellitus. J Clin Diagn Res. 10(12): BC18–BC20 (2016) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5296418/
- Cori CF and Cori GT. The mechanism of epinephrine action IV: The influence of epinephrine on lactic acid production and blood sugar utilization. J Biol Chem, 84: 683 (1929) at http://www.jbc.org/content/84/2/683.full.pdf+html
- Schade DS. The role of catecholamines in metabolic acidosis. Ciba Found Symp, 87:235-53 (1982) at https://www.ncbi.nlm.nih.gov/pubmed/6918290
- Williamson JR. Metabolic effects of epinephrine in the isolated, perfused rat heart. J Biol Chem, 239; 2721-29 (1964) at http://www.jbc.org/content/239/9/2721.full.pdf
- Spigset O and Mjörndal T. Increased glucose intolerance related to digoxin treatment in patients with type 2 diabetes mellitus. Journal of Internal Medicine, Volume 246; Issue 4 (1999) at https://onlinelibrary.wiley.com/doi/full/10.1046/j.1365-2796.1999.00587.x
- Madsen S. Digitalis and diabetes – Case Report. Tidsskr Nor Legeforen nr. 9, 132 (2012) at https://tidsskriftet.no/en/2012/05/digitalis-and-diabetes
- Abdul-Rahima AH, MacIsaac RL, Jhund PS et al. Efficacy and safety of digoxin in patients with heart failure and reduced ejection fraction according to diabetes status: An analysis of the Digitalis Investigation Group (DIG) trial. International Journal of Cardiology 209; 310–316 (2016) at https://www.sciencedirect.com/science/article/abs/pii/S0167527316302984
- Rathore SS, Curtis JP, Wang Y, Bristow MR, Krumholz HM, Association of serum digoxin concentration and outcomes in patients with heart failure, JAMA, 289;871-878 (2003) at https://jamanetwork.com/journals/jama/fullarticle/195990
- Adams KF Jr, Patterson JH, Gattis WA, O Connor CM, Lee CR, Schwartz TA, Gheorghiade M. Relationship of serum digoxin concentration to mortality and morbidity in women in the digitalis investigation group trial: a retrospective analysis. J Am Coll Cardiol. 2;46 (3):497-504; (2005) at https://www.sciencedirect.com/science/article/pii/S0735109705010491
- The Effect of Digoxin on Mortality and Morbidity in Patients with Heart Failure - The Digitalis Investigation Group. N Engl J Med 336:525-533 (1997) at https://www.nejm.org/doi/full/10.1056/nejm199702203360801
- Heart Failure Guidelines from the Heart Failure Society of America. Published at Journal of Cardiac Failure;16:e1-e194: See section 7 (2010) at https://hfsa.org/sites/default/files/media/2015/04/HFSA-2010-HF-Guidelines-Section-07.pdf
- Watanabe AM. Digitalis and the Autonomic Nervous System. JACC Vol. 5; No.5, 35 A - 42A (1985) at https://www.sciencedirect.com/science/article/pii/S0735109785804617?via%3Dihub
- Ferguson DW, Berg WJ, Sanders JS et al. Sympathoinhibitory responses to digitalis glycosides in heart failure patients, Circulation, V80; N1, (1980) at https://www.ahajournals.org/doi/abs/10.1161/01.cir.80.1.65
- Gheorghiade M. Digoxin, a neurohormonal modulator for heart failure? Circulation V84, N5 (1991) at https://www.ahajournals.org/doi/10.1161/01.cir.84.5.2181
- Gheorghiade M, Adams KF, Colucci WS. Digoxin in the Management of Cardiovascular Disorders. Circulation,109; 29592964 (2004) at http://circ.ahajournals.org/content/109/24/2959.long
- Fardin NM, Antonio EL, Montemor JAS et al. Digitoxin improves cardiovascular autonomic control in rats with heart failure. Can J. Pharmacol 94, 18 (2016) at https://pubmed.ncbi.nlm.nih.gov/27082032/
- Gutman Y, Boonyaviroj P. Naunyn Schmiedebergs. Mechanism of inhibition of catecholamine release from adrenal medulla by diphenylhydantoin and by low concentration of ouabain (10 (-10) M). Arch Pharmacol,296(3);293-6 (1977) at https://europepmc.org/article/med/138799
- Calderón-Montaño J, Burgos-Morón E, Lopez-Lazaro M. The Cardiac Glycosides Digitoxin, Digoxin and Ouabain Induce a Potent Inhibition of Glycolysis in Lung Cancer Cells. WebmedCentral CANCER,;4(7);WMC004323 (2013) at https://www.webmedcentral.com/wmcpdf/Article_WMC004323.pdf
- Kypson J, Triner L, Nahas GG. The effects of cardiac glycosides and their interaction with catecholamines on glycolysis and glycogenolysis in skeletal muscle J Pharmacol Exp Ther,164(1); 22-30 (1968) at http://jpet.aspetjournals.org/content/164/1/22.long
- Kenney MJ and Ganta CK. Autonomic Nervous System and Immune System Interactions. Compr Physiol. 4(3): 1177–1200 (2014) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4374437/
- Schneider NFZ, Cerella C, Simões CMO and Diederich M. Anticancer and Immunogenic Properties of Cardiac Glycosides. Molecules 22, 1932 (2017) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6150164/pdf/molecules-22-01932.pdf
- Berbudi A, Rahmadika N, Tjahjadi AI and Ruslamiet R. Type 2 Diabetes and its Impact on the Immune System. Curr Diabetes Rev. 16(5), 442–449 (2020) at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7475801/
- O’Hearn M, Liu J, Cudhea F, Micha R, and Mozaffarian D. Coronavirus Disease 2019 Hospitalizations Attributable to Cardiometabolic Conditions in the United States: A Comparative Risk Assessment Analysis. Journal of the American Heart Association. 10:e019259 (2021) at https://www.ahajournals.org/doi/10.1161/JAHA.120.019259
- Monteiro CETB. Covid-19: Treating Cause and Effects - “Autonomic Dysfunction, the Immune System and Lactic Acidosis”. Letter to the Editor of Positive Health Online published in issue 263, [2020] at http://www.positivehealth.com/article/letters-to-the-editor/letters-to-theeditor-issue-263 . A copy of the Letter can also be found at http://infarctcombat.org/Covid-19.LettertotheEditorPHO.pdf
- Yuchen Pan, Zhiyao Yu, Yuan Yuan, et al. Alteration of Autonomic Nervous System Is Associated With Severity and Outcomes in Patients With COVID-19”, published in Front Physiol. [2021] at https://www.frontiersin.org/articles/10.3389/fphys.2021.630038/full
- Martha JW, Wibowo A and Pranata R. Prognostic value of elevated lactate dehydrogenase in patients with COVID-19: a systematic review and meta-analysis', Postgrad Med J [2021] at https://pmj.bmj.com/content/postgradmedj/early/2021/01/14/postgradmedj-2020-139542.full.pdf
- Siniorakis E, Arvanitakis SBM, Katsianis and Elkouris M. Atrial fibrillation and flutter in patients hospitalized for COVID-19: The challenging role of digoxin. Journal of Cardiovascular Electrophysiology (2021) at https://onlinelibrary.wiley.com/doi/10.1111/jce.14894
Comments:
-
No Article Comments available